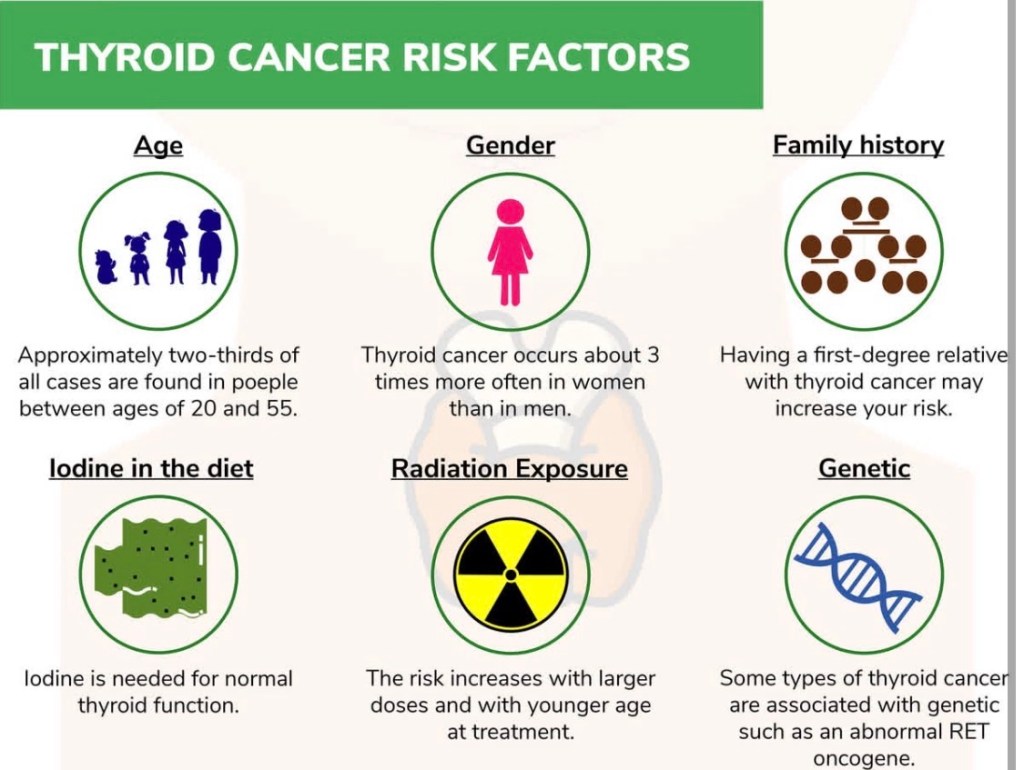
Age plays an important role in how thyroid cancer behaves, how it is staged, and how it is treated.
👶 Thyroid cancer in younger patients
More common in women Often presents with lymph node involvement Tumors may look aggressive on imaging 👉 Despite this, prognosis is excellent
✔️ Patients under 55 years are staged differently
✔️ Even with lymph nodes, survival rates exceed 98–99%
✔️ Treatment focuses on curing disease while preserving quality of life
👴 Thyroid cancer in older patients
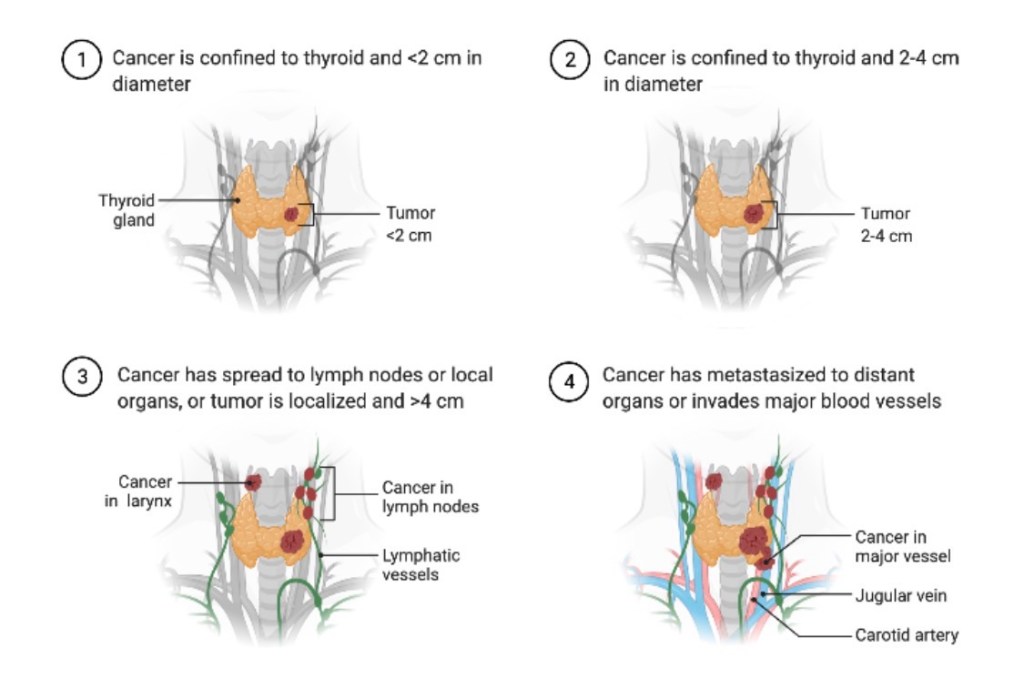
Less common, but tumors may be biologically more aggressive Higher likelihood of: Extrathyroidal extension Distant metastases Higher-stage disease Outcomes are still often very good, but treatment may need to be more comprehensive
⚖️ Why age matters
Age helps determine:
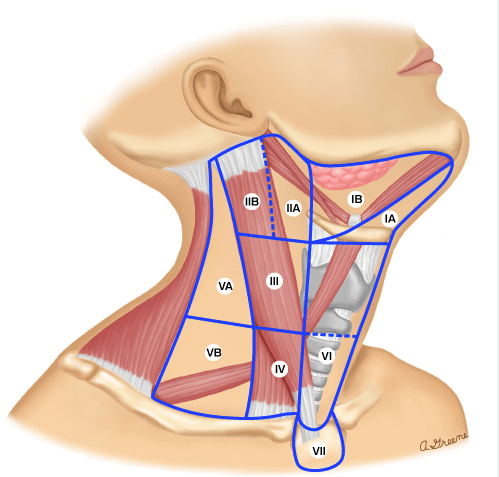
AJCC stage Expected prognosis Intensity of treatment and follow-up
🧠 Important clarification:
Age alone does not determine outcome.
➡️ Tumor biology, pathology, and response to treatment matter most.
🦋 What this means for patients
Thyroid cancer is not the same disease in every patient.
The goal is personalized, risk-adapted care—not one-size-fits-all treatment.
👨⚕️ Dr. Rodrigo Arrangoiz, MD
Surgical Oncologist – Thyroid, Head & Neck, Breast
Mount Sinai Medical Center
📌 Take-home message:
Young patients do extremely well.
Older patients still have excellent outcomes with expert, individualized care.
📚 References
AJCC Cancer Staging Manual, 8th Edition Haugen BR et al. ATA Guidelines for Differentiated Thyroid Cancer. Thyroid Tuttle RM et al. Risk-adapted management of thyroid cancer. Lancet Diabetes Endocrinol