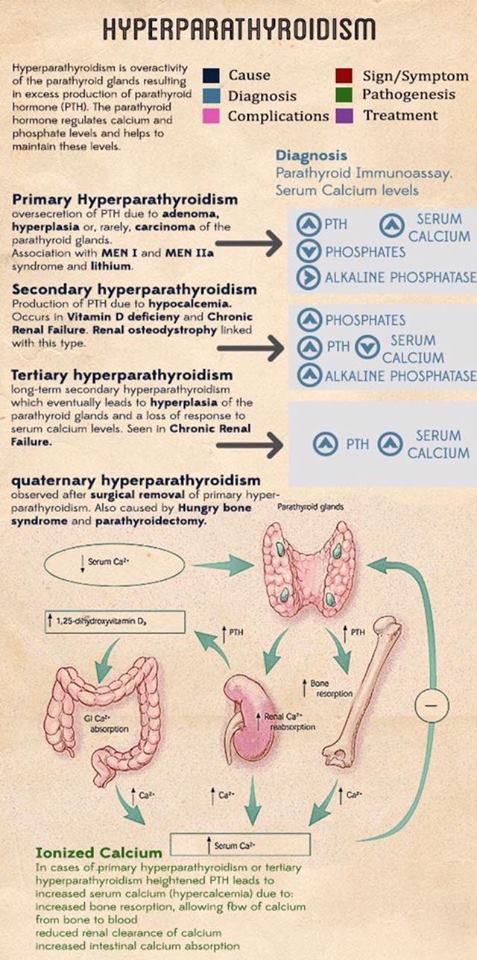
- Despite what most of the literature reports:
- PHPT is symptomatic in more than 95% of the cases if proper attention is payed to the subtle symptoms and signs that this disease can produce due to the fluctuating calcium levels
- The “classic” pentad of:
- Kidney stones
- Painful bones
- Abdominal groans
- Psychic moans. and
- Fatigue overtones
- Are rarely seen today since the advent and general use of automated blood analyzers in the early 1970s
- At this point in time most patients present with:
- Fatigue (# 1 symptom)
- General malaise
- Decrease levels of energy
- Anxiety
- Irritability leading to decrease social interaction
- Depression (10% of cases)
- Memory loss
- Decrease concentration
- Decrease ability to learn new things
- Decrease ability to complete daily tasks at home
- Decrease ability to complete daily tasks at work
- Decrease social interaction
- Insomnia
- Arthralgia’s (32% of the cases)
- Myalgia’s (14% to 41% of the cases)
- Bone pain
- Muscle weakness (specially proximal muscle groups)
- Intermittent headaches
- Polydipsia
- Polyuria
- Nocturia
- Nausea (24% of the cases)
- Anorexia (15% of the cases)
- Non-specific abdominal pain
- Heartburn (30% of the cases)
- Constipation (33% of the cases)
- Palpitations, arrhythmias (usually atrial fibrillation)
- Elevated blood pressure
- Thinning of the hair (specially in women in the frontal region)
- Pruritus
- Patients with PHPT also tend to score lower than healthy controls when evaluated by general multidimensional health assessment tools:
- Such as the Medical Outcomes Study Short-Form Health Survey (SF-36) and other specific questionnaires
- PHPT that is truly “asymptomatic” is a rare occurrence:
- Seen in less than 5% of patients:
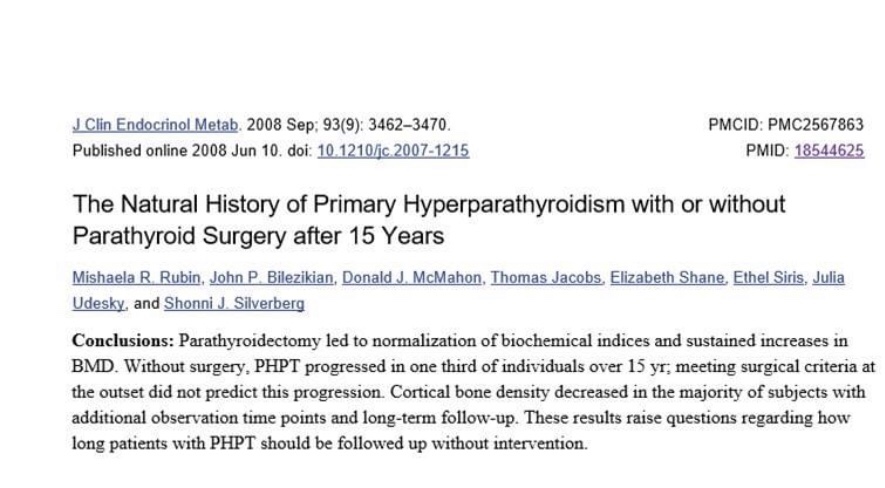
- This is important when talking about management based on current guidelines
- Seen in less than 5% of patients:
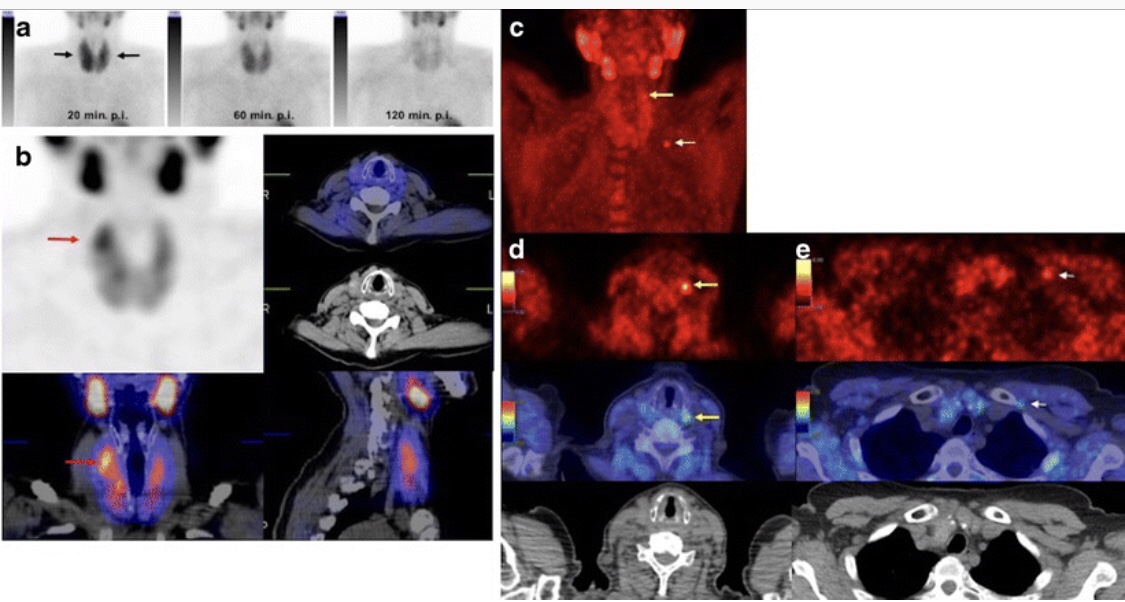
- Patients with PHPT have some degree of renal dysfunction or symptoms in approximately 80% of the cases. The renal manifestations implicated with PHPT are decreased glomerular filtration rate, hypercalciuria, nephrolithiasis, nephrocalcinosis, impaired urinary concentrating ability sometimes leading to polyuria, polydipsia, and nocturia, reduced fractional phosphate reabsorption leading to hypophosphatemia, and increased urinary exertion of magnesium [66]. Nephrolithiasis was previously reported in approximately40% to 80% of patients [77], but now occur only in about 20% to 25% of the cases [78]. The pathophysiology is thought to be related to the filtered load of calcium in the glomerulus that increases proportionately with the degree of hypocalcaemia [79]. Most renal stones in patients with PHPT are composed of calcium oxalate, although slightly alkaline urine may favor the precipitation of calcium phosphate stones [79,80]. Stone formers are more likely to be hypercalciuric, but less than one-third of the hypercalciuric patients with PHPT actually develop renal stones [80]. Hypercalciuria is not a predictor of nephrolithiasis in patients with PHPT and is no longer considered as an indication for surgery [81]. At the present
- Skeletal manifestations includingosteopenia, osteoporosis, and osteitis fibrosacystica, are found in approximately 15% of patients with PHPT [88,89]. PHPT is linked with a reduction in bone mineral density (BMD), particularly in the cortical bone, such as in the distal third of the radius [88,89]. In the lumbar region, composed all most exclusively by trabecular bone, and in the femoral region, composed by cortical and trabecular bone, the decrease in BMD is less severe . Osteitis fibrosacystica, a skeletal manifestation that is rarely seen today (seen in less than five percent of patients with PHPT), is caused by an increase in bone turnover and can be determined by finding an elevated serum alkaline phosphatase level [91]. The radiologic findings seen in patients with PHPT with bone disease are characterized by subperiosteal resorption (most obvious on the radial aspect of the middle phalanx of the second and third fingers), bone cysts, and tufting of the distal phalanges [92], which are best evaluated on plain x-rays of the hands. Brown or osteoclastic tumors (accumulations of osteoclasts and fibrous tissue) and bone cysts also may be present [93]. Brown tumors have a slightly greater incidence in PHPT than in secondary HPT (3% versus 2%) [94]. In patients with chronic kidney disease, persistent and excessive urinary calcium elimination can lower serum calcium level and lead to an increase in PTH secretion. This results in mobilization of calcium from the bones through rapid osteoclastic turnover of bone to maintain normal serum calcium levels . In regions where bone loss is exceptionally fast, hemorrhage, and reparative granulation tissue, with active, vascular, proliferating fibrous tissue may replace the normal marrow contents, resulting in a brown tumor. Hemosiderin imparts the brown color(hence the name of the lesions). The skull also may be affected and appears mottled with a loss of definition of the inner and outer cortices . Patients with normal serum alkaline phosphatase levels almost never have clinically apparent osteitis fibrosacystica. Bone disease correlates with serum PTH and vitamin D levels. The most frequent gastrointestinal manifestations of PHPT are constipation, heartburn, nausea and anorexia that occur in 33%, 30%, 24% and 15% of cases, respectively [69]. A significant reduction in patient symptoms is seen after parathyroidectomy. The precise Pathophysiology is not fully known. Variations in gene expression secondary to sustained stimulation of PTH
- Nephrocalcinosis, which refers to renal parenchymal calcification, is found in less than five percent of patients and is more likely to lead to renal dysfunction [82]. The incidence of hypertension is variable, anywhere between 30% to 50% of patients with PHPT. Hypertension appears to be more common in older patients and correlates with the magnitude of renal dysfunction and, in contrast to other symptoms, is least likely to improve after parathyroidectomy [84]. Another plausible explanation of the origin of hypertension in patients with PHPT is the synthesis of parathyroid hypertensive factor that triggers an increase in blood pressure. The elevated levels of PTH is also linked with the disruption in the renin-angiotensin- aldosterone system.