Follicular thyroid cancer (FTC) accounts for ~10–15% of thyroid cancers. While less common than papillary thyroid cancer, it is still highly treatable, especially when diagnosed early.
🧠 Key characteristics of FTC
Tends to spread through the bloodstream rather than lymph nodes Can metastasize to lungs or bones (uncommon, usually in higher-risk disease) Often appears similar to benign nodules on ultrasound Diagnosis depends on capsular and/or vascular invasion, which cannot be confirmed by FNA alone
🔍 How is FTC diagnosed?
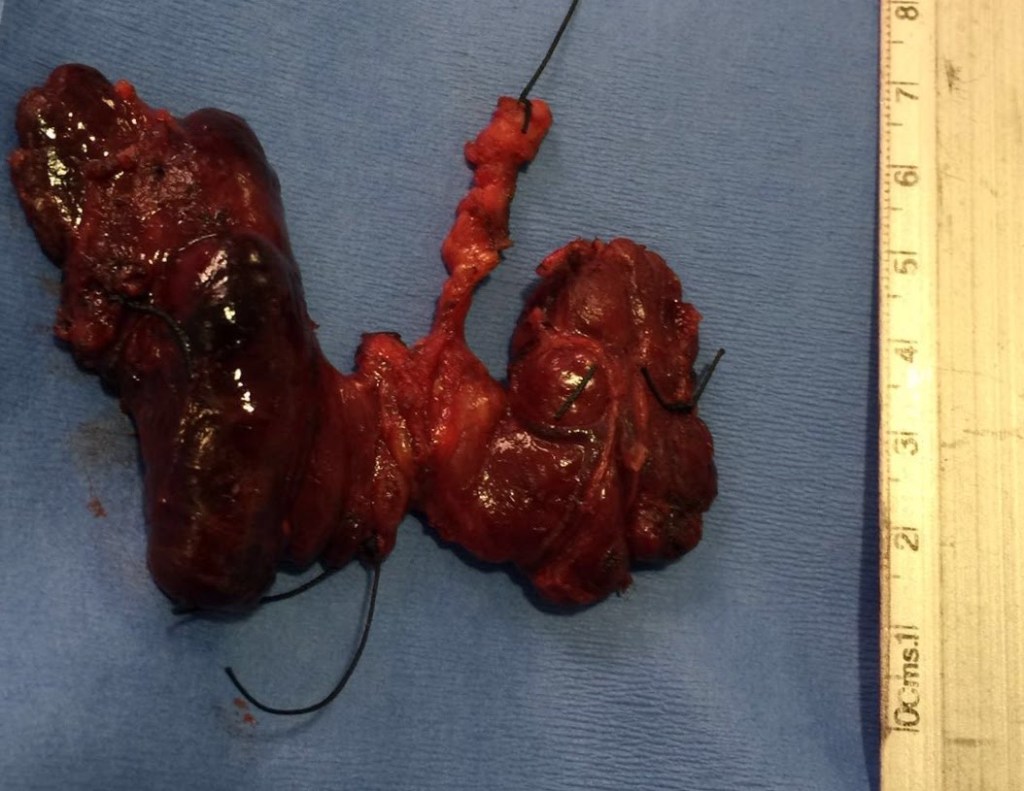
Ultrasound and FNA may suggest a follicular neoplasm Definitive diagnosis requires surgery and full histologic evaluation Pathology distinguishes: Minimally invasive FTC Widely invasive FTC
⚖️ How is follicular thyroid cancer treated?
Management is risk-adapted and may include:
Thyroid lobectomy for minimally invasive, low-risk tumors Total thyroidectomy for higher-risk disease Radioactive iodine selectively for tumors with vascular invasion or metastases Long-term surveillance with thyroglobulin and imaging
📈 Prognosis
Excellent outcomes for minimally invasive FTC Prognosis depends on: Degree of vascular invasion Tumor size Patient age
🦋 Early, appropriate management leads to very high cure rates.
👨⚕️ Dr. Rodrigo Arrangoiz, MD
Surgical Oncologist – Thyroid, Head & Neck, Breast
Mount Sinai Medical Center
📌 Take-home message:
Follicular thyroid cancer often requires surgery for diagnosis, but when managed correctly, outcomes are excellent.
📚 References
Haugen BR et al. ATA Guidelines for Differentiated Thyroid Cancer. Thyroid Lloyd RV et al. WHO Classification of Tumours of Endocrine Organs. Tuttle RM et al. Risk-adapted management of differentiated thyroid cancer. Lancet Diabetes Endocrinol