- The sequence (seconds → minutes):
- Vascular injury and vasoconstriction:
- Neurogenic reflex + endothelin:
- Transient narrowing:
- Slows flow and exposes subendothelial collagen and vWF
- Transient narrowing:
- Neurogenic reflex + endothelin:
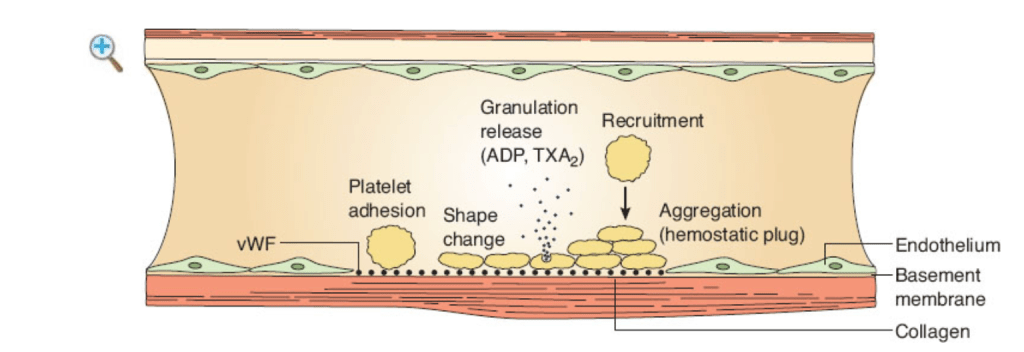
- Platelet adhesion (to the wound):
- vWF anchored on exposed collagen binds GP Ib-IX-V on platelets (high-shear arterial beds):
- Platelet membrane glycoprotein Ib–IX–V complex:
- The major von Willebrand factor (vWF) receptor:
- That mediates initial platelet adhesion:
- At sites of vascular injury (especially high-shear arteries)
- That mediates initial platelet adhesion:
- The major von Willebrand factor (vWF) receptor:
- Platelet membrane glycoprotein Ib–IX–V complex:
- Direct collagen binding via GP Ia/IIa (α2β1) and GP VI:
- Complements adhesion
- vWF anchored on exposed collagen binds GP Ib-IX-V on platelets (high-shear arterial beds):
- Activation and shape change:
- Cytoskeleton rearranges:
- Discoid → spiky:
- ↑ surface area:
- Phosphatidylserine flips outward
- ↑ surface area:
- Discoid → spiky:
- Platelets synthesize / release mediators:
- Dense granules:
- ADP, ATP, Ca²⁺, serotonin
- Alpha granules:
- vWF, fibrinogen, factor V, fibronectin, P-selectin, PDGF, TGF-β
- TxA₂ is generated via:
- COX-1 (aspirin target)
- Dense granules:
- Cytoskeleton rearranges:
- Recruitment (amplification):
- ADP → P2Y12/P2Y1, TxA₂ (TP receptor), thrombin (PAR-1 / PAR-4):
- Amplify activation on nearby platelets
- Ca²⁺ is essential for signaling and integrin activation
- ADP → P2Y12/P2Y1, TxA₂ (TP receptor), thrombin (PAR-1 / PAR-4):
- Aggregation (hemostatic plug formation):
- Activated GP IIb/IIIa (αIIbβ3) undergoes conformational change:
- Fibrinogen bridges adjacent platelets:
- Primary hemostatic plug
- Fibrinogen bridges adjacent platelets:
- Leukocytes tether via P-selectin:
- Adding stability
- Handoff to secondary hemostasis (minutes):
- Tissue factor (injured cells) plus factor VII:
- Activate factor X :
- Factor X plus factor V:
- Convert prothrombin (factor II) to thrombin:
- Converts fibrinogen to fibrin polymer:
- Factor XIII crosslinks fibrin:
- Stabilizing the platelet plug
- Factor XIII crosslinks fibrin:
- Converts fibrinogen to fibrin polymer:
- Convert prothrombin (factor II) to thrombin:
- Factor X plus factor V:
- Activate factor X :
- Tissue factor (injured cells) plus factor VII:
- Activated GP IIb/IIIa (αIIbβ3) undergoes conformational change:
- Vascular injury and vasoconstriction:
- Why surgeons care (pattern recognition):
- Primary (platelet) defects:
- Mucocutaneous bleeding, oozing from raw surfaces, petechiae, immediate post-incision bleeding
- PT / PTT often normal
- Secondary (coagulation) defects:
- Delayed re-bleeding, deep tissue / hematoma, hemarthrosis
- Primary (platelet) defects:
- Drugs and diseases mapped to the steps:
- Adhesion:
- ↓ vWF (von Willebrand disease) → poor GP Ib-vWF “tether”:
- DDAVP can ↑ endothelial vWF release (Type 1 vWD, some qualitative defects)
- ↓ vWF (von Willebrand disease) → poor GP Ib-vWF “tether”:
- Activation:
- Aspirin / NSAIDs → block COX-1 → TxA₂ (qualitative dysfunction)
- Uremia, hypothermia, acidosis, hemodilution / CPB:
- Global platelet dysfunction
- DDAVP helps in uremia
- Recruitment:
- P2Y12 inhibitors (clopidogrel, prasugrel, ticagrelor) blunt ADP signaling
- Aggregation:
- Gp IIb/IIIa antagonists (eptifibatide/tirofiban) block fibrinogen bridging
- Glanzmann thrombasthenia (GP IIb/IIIa deficiency):
- Severe aggregation defect
- Bernard–Soulier (GP Ib deficiency):
- Adhesion failure; giant platelets
- Adhesion:
- Practical peri-op numbers (rules of thumb):
- Platelet count targets (institutional policies vary):
- Most non-neurosurgical / non-ocular operations:
- ≥ 50k/µL
- Neuraxial, intracranial, posterior eye:
- ≥ 80 to 100k/µL
- Ongoing microvascular free-flap or diffuse oozing often needs:
- > 75 to 100k/µL and intact function
- Most non-neurosurgical / non-ocular operations:
- Apheresis platelets:
- Typically ↑ count by ~ 30 to 50k/µL in a 70-kg adult
- Coordinate any antiplatelet interruption with cardiology (especially recent stents):
- If drugs cannot be stopped, plan local / topical strategies and consider point-of-care testing
- Platelet count targets (institutional policies vary):
- OR playbook for platelet-type bleeding:
- Pre-op:
- Focused history (mucosal bleeding, easy bruising), meds (aspirin, P2Y12), renal function
- Consider PFA-100/VerifyNow/TEG-PlateletMapping if results will change management
- Intra-op:
- Local control:
- Meticulous pressure, bipolar, vessel loops; topical hemostats (thrombin, gelatin sponge, oxidized cellulose, collagen matrix, fibrin sealant)
- Antifibrinolytics:
- Tranexamic acid (IV / topical) particularly helpful on mucosal fields (head and neck, oral cavity)
- Maintain normothermia, ionized Ca²⁺, pH > 7.2; avoid hemodilution
- If on aspirin / P2Y12 with urgent bleeding:
- Platelet transfusion can overcome irreversible blockade (earlier works better for aspirin than ticagrelor); weigh thrombosis risk
- DDAVP for vWD Type 1 or uremic dysfunction (watch Na⁺; tachyphylaxis after 1 to 2 doses)
- Local control:
- Post-op:
- Control blood pressure, avoid NSAIDs, continue local antifibrinolytics when helpful (e.g., pledgets / mouthwash in mucosal cases), and reassess platelet count / function if oozing persists
- Pre-op:
- Quick differentials when the field won’t dry:
- Normal PT / PTT, low platelets or recent antiplatelet use → primary hemostasis problem
- Prolonged PT / PTT, normal platelets → secondary hemostasis issue (think tissue factor pathway, anticoagulants)
- Everything “normal,” but diffuse oozing → platelet dysfunction (uremia, hypothermia, CPB, meds) ± hyperfibrinolysis (consider TXA, fibrinogen / cryoprecipitate guided by TEG/ROTEM)