- Clinical Management Principles:
- Dictionary and Definitions:
- Several terms are utilized throughout the guidelines in different sections and recommendations
- Dictionary and Definitions:
- Important definitions used by the committee are included below:
- General definitions:
- Active surveillance:
- The ongoing observation or active monitoring of a known or suspected primary, intrathyroidal, low-risk DTC with serial imaging as an alternative to upfront surgical intervention
- This is a type of expectant management and is only appropriate for a subset of low-risk DTCs (see Recommendation 11)
- This does not pertain to persistent or recurrent thyroid cancer, in which case the term “monitoring” is employed (see below)
- Some proportion of patients who undergo active surveillance may be recommended to pursue thyroid surgery if there is concern for disease progression or based on patient preference
- Disease monitoring:
- Monitoring for biochemical (elevated level of serum Tg) and / or structural persistence or recurrence of disease (as confirmed by imaging and / or biopsy) following the diagnosis and initial treatment (surgery – RAI) of thyroid cancer
- It is deployed to evaluate patients for disease progression and inform the type and timing of interventions deemed appropriate
- Response to therapy:
- Response assessment is performed after intervention:
- Either for initial or clinically persistent / recurrent disease (see Recommendation 29 and Table 9 of the ATA 2025 Guidelines)
- Excellent response:
- No biochemical or structural evidence of persistent thyroid cancer (i.e., remission)
- Indeterminate response:
- The presence of nonspecific findings on imaging; mildly elevated serum Tg levels; or positive, but stable or declining, anti-Tg antibody (TgAb) levels in persons who have undergone total thyroidectomy with or without RAI
- Most patients in this category prove to have a “good” clinical response to therapy, especially if they have a low risk of clinical recurrence, and findings are nonspecific
- However, those at intermediate or high risk of clinical recurrence based on histopathologic and staging characteristics in this category:
- May have higher rates of recurrence
- Biochemically incomplete response:
- Elevated serum Tg concentrations or rising TgAb levels without radiological evidence of structural recurrence in persons who have undergone total thyroidectomy with or without RAI
- Structurally incomplete response:
- Structural evidence of disease recurrence (by imaging or biopsy), usually in conjunction with elevated Tg and / or TgAb levels
- Persistent or recurrent disease:
- See Recommendation 29 and Table 9 of the ATA 2025 Guidelines
- Clinically persistent disease:
- Biochemical or structural evidence of disease within 90 days of initial therapy (or intervention for persistent disease)
- Clinically recurrent disease:
- Biochemical or structural disease subsequently identified in patients previously deemed to have an excellent response following therapy
- Clinically recurrent disease likely represents progression of residual disease that is below the lower limits of detection
- Risk of recurrence:
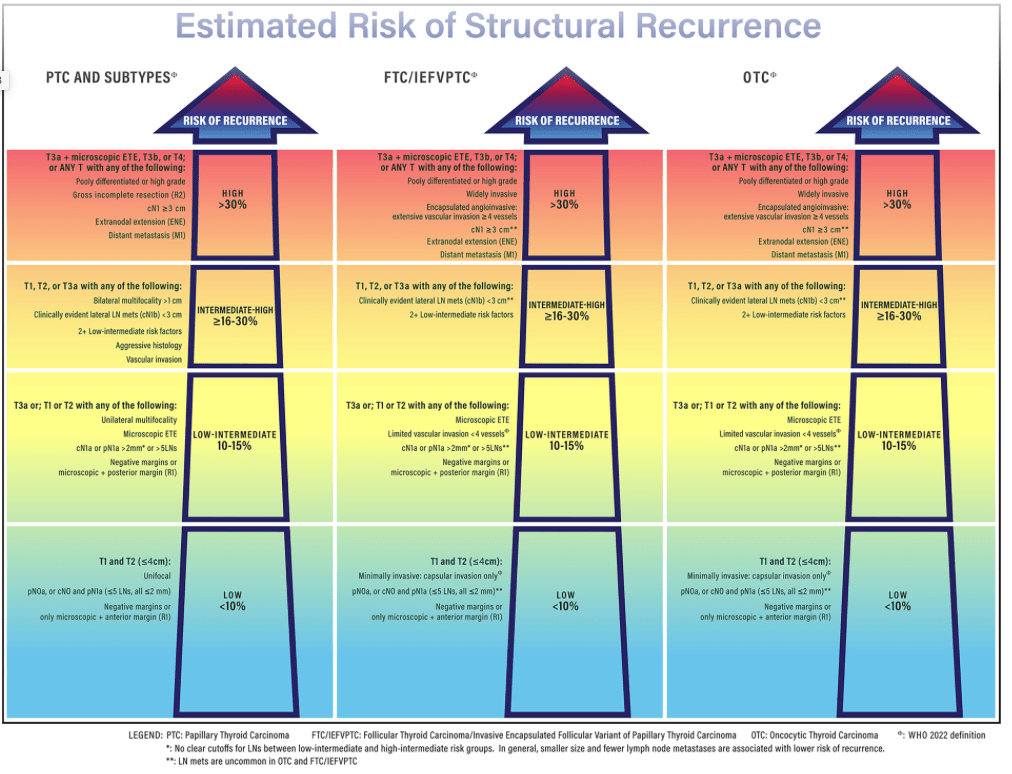
- They use the term “recurrence” to mean clinical recurrence, recognizing that most recurrences reflect growth of residual disease to clinically detectable levels (Figure )
- An overall assessment of risk of biochemical or structural recurrence determined by incorporating a combination of factors:
- Histopathologic characteristics of the resected tumor, American Joint Committee on Cancer (AJCC) staging, imaging, molecular analysis of tumor, and response to therapy at subsequent evaluation
- For the purpose of these guidelines, categories are designated as:
- Low (< 10%) risk of recurrence
- Low Intermediate (10% to 15%) risk of recurrence
- Intermediate-high (≥ 16% to 30%) risk of recurrence
- High (> 30%) risk of recurrence
- Active surveillance:
- General definitions:
- Treatment Definitions:
- Extent of surgery definitions (ATA website definitions):
- Total thyroidectomy:
- Surgical removal of the entire thyroid gland
- Near-total thyroidectomy:
- Intended extent of resection for thyroid cancer is total thyroidectomy:
- But a small remnant may be left for a specific reason (usually confidence in nerve preservation)
- Intended extent of resection for thyroid cancer is total thyroidectomy:
- Lobectomy or hemithyroidectomy with or without isthmusectomy:
- Surgical removal of one lobe (half) of the thyroid with or without the isthmus
- Subtotal thyroidectomy:
- Surgical removal of almost all of the thyroid gland, leaving 3 to 5 g of thyroid tissue with the intent of maintaining adequate thyroid hormone production:
- This operation is not recommended if the diagnosis of thyroid cancer is known preoperatively
- Completion thyroidectomy:
- Surgical removal of the remnant thyroid tissue following procedures of less than total or near-total thyroidectomy
- Surgical removal of almost all of the thyroid gland, leaving 3 to 5 g of thyroid tissue with the intent of maintaining adequate thyroid hormone production:
- Total thyroidectomy:
- Extent of lymphadenectomy definitions:
- Central neck dissection:
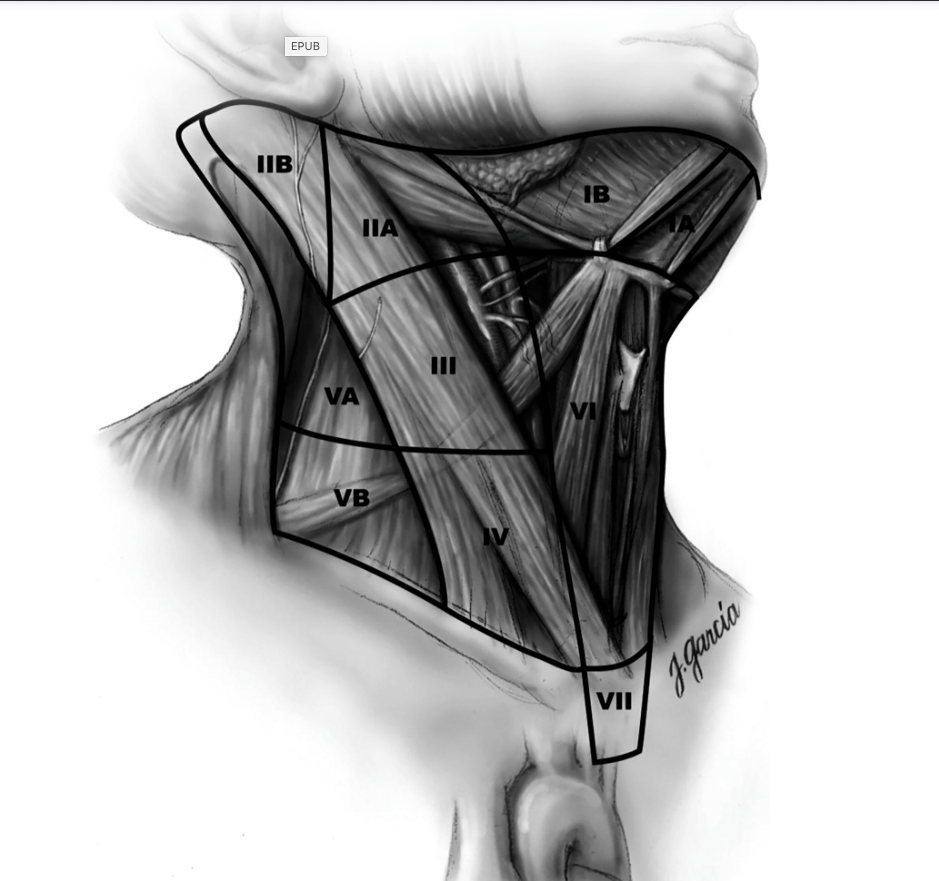
- Central neck lymph nodes include Levels VI and VII (Figure)
- Central neck dissection is a comprehensive removal of pretracheal and prelaryngeal lymph nodes, along with at least one paratracheal nodal basin
- It can be unilateral or bilateral; the laterality and extent of dissection should be documented at the time of operation in addition to surgical intent (therapeutic vs. prophylactic)
- Therapeutic neck dissection:
- It implies that metastatic nodal disease is apparent clinically preoperatively or intraoperatively by examination and / or imaging, cN1a
- Prophylactic neck dissection:
- It implies that no metastatic nodes are detected by examination or imaging preoperatively or intraoperatively, cN0
- Lateral neck dissection:
- Full compartment dissection of the lateral cervical neck lymph nodes in Levels IIA, III, IV, and VB ipsilateral to the tumor and performed for clinical evidence of metastatic involvement
- Dissection of Levels I, IIB, and VA are not regularly performed but can be considered based on findings suggestive of metastatic disease in these compartments (Figure)
- Completeness of surgical resection:
- The goal of surgery is to remove safely as much thyroid cancer as possible
- To define the completeness of resection, the AJCC created definitions that are used in these guidelines to facilitate communications
- An R0 resection:
- Means that the surgical margin is microscopically negative for residual tumor
- An R1 resection:
- Means that there is no residual macroscopic tumor but that microscopically positive margins still demonstrate the presence of tumor
- An R2 resection:
- Means that gross (macroscopic) disease remains post-surgery
- Central neck dissection:
- Extent of surgery definitions (ATA website definitions):
- 131I, RAI administration definitions:
- Remnant ablation:
- RAI administration to destroy benign remnant thyroid tissue following total or near-total thyroidectomy
- Adjuvant therapy:
- RAI administration to destroy suspected (but not identified) remaining thyroid cancer following total or near-total thyroidectomy
- Therapeutic treatment:
- RAI administration to treat known residual or recurrent thyroid cancer, either initially or with subsequent progression of thyroid cancer after total or near-total thyroidectomy
- Thyrotropin suppression therapy:
- Use of thyroid hormone to suppress serum thyrotropin (TSH) concentrations below the normal range based on the risk of recurrence and / or response to therapy
- Remnant ablation:

