- Differential Diagnosis of Hypercalcemia:
- Primary hyperparathyroidism:
- Solitary adenoma:
- 85% to 90% of the cases
- Multigland hyperplasia:
- 3% of the cases
- Doble adenoma:
- 6% to 9% of the cases
- Triple adenoma:
- 0.3% of the cases
- Solitary adenoma:
- Secondary hyperparathyroidism
- Tertiary hyperparathyroidism
- Familial hypocalciuric hypercalcemia
- Medications:
- Lithium
- Hydrochlorothiazide
- Malignancy:
- Parathyroid carcinoma
- Multiple myeloma
- Tumors producing PTH-related peptide:
- Ovarian cancer
- Lung cancer
- Acute or chronic leukemia
- Sarcoidosis
- Thyrotoxicosis
- Paget disease
- Increased intake:
- Milk-alkali syndrome
- Vitamin A toxicity
- Vitamin D toxicity
- Primary hyperparathyroidism:
- Primary hyperparathyroidism (PHPT):
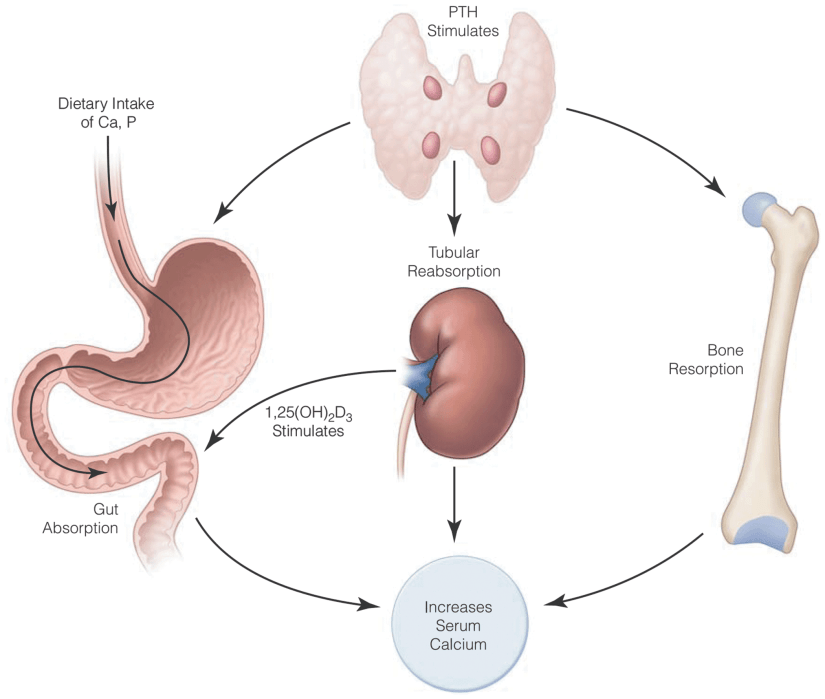
- Is caused by an inappropriate, autonomous secretion of parathyroid hormone (PTH) by the parathyroid gland (s), which leads to an elevated serum calcium concentration or wide variations of the serum calcium concentration.
- Single gland disease:
- Caused by a single, enlarged, overactive gland, is found in 85% to 90% of cases.
- Multiple gland disease occurs in 10% to 15% of the cases:
- Multiple gland disease may consist of:
- Double adenomas (6% to 9% of the cases)
- Four-gland hyperplasia (3% of the cases)
- Three enlarged and one normal appearing gland (0.3% of the cases).
- Because asymmetric hyperplasia is common, it is difficult to distinguish between multiple adenomas and hyperplasia and the term multiple gland disease is preferred.
- Multiple gland disease may consist of:
- PHPT in the United States usually presents quite early, often when hypercalcemia is noted during routine laboratory testing.
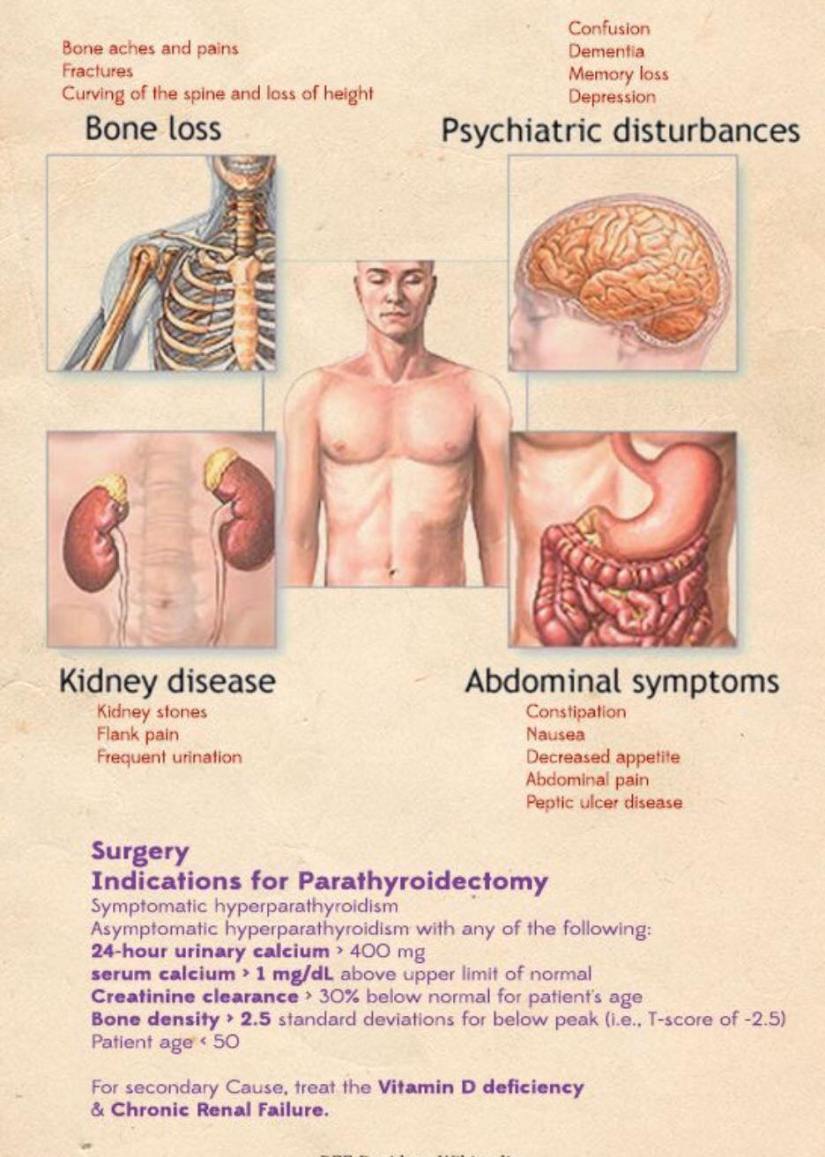
- Signs may include:
- Nephrolithiasis, decreased bone density, and fragility fractures, and subjective symptoms may include fatigue, cognitive changes, depression, constipation and other gastrointestinal complaints, musculoskeletal pain, nocturia, and rarely pruritus:
- Many patients may appear asymptomatic:
- A detailed history often uncovers symptoms:
- 95% of the cases have symptoms when appropriate history is taken.
- The recently revised guidelines for asymptomatic PHPT include a more extensive evaluation of the skeletal and renal systems.
- 95% of the cases have symptoms when appropriate history is taken.
- A detailed history often uncovers symptoms:
- Many patients may appear asymptomatic:
- Nephrolithiasis, decreased bone density, and fragility fractures, and subjective symptoms may include fatigue, cognitive changes, depression, constipation and other gastrointestinal complaints, musculoskeletal pain, nocturia, and rarely pruritus:
- A family history of endocrine disorders should be investigated:
- As hyperparathyroidism alone can be familial or can present as a component of multiple endocrine neoplasia (MEN) types 1 and 2A.






Rodrigo Arrangoiz MS, MD, FACS cirujano de tumores de cabeza y cuello / cirugia endocrina miembro del equipo de Mount Sinai Medical Center experto en el manejo del hiperparatiroidismo primario.
Entrenamiento:
-
Cirugia general y gastrointestinal:
• Michigan State University:
• 2004 al 2010
• Cirugia oncológica / tumores de cabeza y cuello / cirugia endocrina:
• Fox Chase Cancer Center (Filadelfia):
• 2010 al 2012
• Maestria en ciencias (Clinical research for healthprofessionals):
• Drexel University (Filadelfia):
• 2010 al 2012
• Cirugia de tumores de cabeza y cuello / cirugiaendocrina
• IFHNOS / Memorial Sloan Kettering Cancer Center:
• 2014 al 2016
#Arrangoiz
#CirugiadeTumoresdeCabezayCuello
#CirugiaEndocrina
#CirugiaOncologica
#HeadandNeckSurgery
#EndocrineSurgery
#SurgicalOncology
#Hiperparatiroidismo
#Hyperparathyroidsim
#MountSInaiMedicalCenter
#MSMC
#Mexico #Miami


