- Secondary hyperparathyroidism:
- Is overproduction of parathyroid hormone (PTH):
- Due to a nonparathyroid cause:
- Usually a result of renal failure
- Due to a nonparathyroid cause:
- Renal failure decreases the production of 1,25(OH)2 D3:
- Impairing intestinal absorption of calcium:
- Leading to hypocalcemia:
- Which increases PTH secretion by the parathyroid glands:
- Leading to diffuse or nodular hyperplasia
- Which increases PTH secretion by the parathyroid glands:
- Leading to hypocalcemia:
- Impairing intestinal absorption of calcium:
- Hyperphosphatemia:
- From decreased renal excretion also contributes to PTH secretion:
- The resulting calcium level is low or normal
- From decreased renal excretion also contributes to PTH secretion:
- Less common causes of secondary hyperparathyroidism include:
- Osteomalacia
- Long-term lithium therapy
- Vitamin D deficiency
- Malabsorption syndromes
- Secondary hyperparathyroidism has beenv increasingly described following bariatric surgery:
- Most commonly Roux-en-Y gastric bypass and duodenal switch:
- Due to prolonged vitamin D deficiency:
- It occurs despite vitamin D replacement
- Due to prolonged vitamin D deficiency:
- Most commonly Roux-en-Y gastric bypass and duodenal switch:
- Is overproduction of parathyroid hormone (PTH):
- The pathophysiology of secondary hyperparathyroidism:
- Is multifactorial and can result from:
- Phosphorous retention
- Altered vitamin D metabolism and resistance
- Altered metabolism of PTH
- Impaired calcemic response to PTH
- Possible genetic mutations
- Is multifactorial and can result from:
- The condition most commonly occurs in patients:
- With a history of chronic renal failure
- Gastric bypass:
- Has also been an increasingly recognized cause of altered vitamin D metabolism
- Patients will commonly have:
- An elevated PTH level and normal or low serum calcium:
- In such a setting, vitamin D levels should be measured:
- If low, treated for a minimum of 6 weeks with supplemental vitamin D
- In such a setting, vitamin D levels should be measured:
- An elevated PTH level and normal or low serum calcium:
- Secondary hyperparathyroidism:
- Is most commonly managed medically with the use of:
- Calcimimetic agents:
- For example cinacalcet
- Phosphate binders
- Adequate calcium intake
- Vitamin D replacement
- Calcimimetic agents:
- Is most commonly managed medically with the use of:
- Cinacalcet:
- Works by binding the calcium-sensing receptors on the chief cells of the parathyroid gland:
- Increasing its sensitivity to extracellular calcium
- Works by binding the calcium-sensing receptors on the chief cells of the parathyroid gland:
- Surgical treatment is indicated in patients with:
- Renal osteodystrophy
- Calciphylaxis:
- Calciphylaxis is a rare complication of secondary hyperparathyroidism resulting in acute deposition of calcium in tissues and skin necrosis:
- That may lead to a systemic inflammatory response:
- It is associated with a high rate of mortality (87 to 93%)
- That may lead to a systemic inflammatory response:
- Calcium phosphate product of ≥ 70
- Soft tissue calcium deposition and tumoral calcinosis
- Calcium level greater than 11 mg/dL with an inappropriately high level of PTH
- Calciphylaxis is a rare complication of secondary hyperparathyroidism resulting in acute deposition of calcium in tissues and skin necrosis:
- Renal osteodystrophy:
- Is a major issue in hemodialysis patients:
- The aluminum present in the dialysate bath:
- Accumulates in the bone:
- Contributes to the development of osteomalacia
- Accumulates in the bone:
- The aluminum present in the dialysate bath:
- Is a major issue in hemodialysis patients:
- Osteitis fibrosa cystica:
- A type of renal osteodystrophy:
- Is characterized by marrow fibrosis and increased bone turnover
- Bone cysts, osteopenia, and decreased bone strength develop
- To halt the progression of this disease process:
- These patients with secondary hyperparathyroidism are treated surgically
- A type of renal osteodystrophy:
- Calciphylaxis:
- Is a rare vascular disorder:
- In which calcium is deposited in the media of small- to medium-sized arteries
- As a result, ischemic damage:
- To the dermal and epidermal structures develops
- As a result, ischemic damage:
- In which calcium is deposited in the media of small- to medium-sized arteries
- The ulcerated lesions:
- Are extremely painful and can become infected with subsequent sepsis, and eventually death
- Patients with early signs of calciphylaxis:
- Should undergo an urgent parathyroidectomy:
- Although there is some evidence that aggressive management of serum calcium and parathyroid levels:
- With cinacalcet may be beneficial
- Although there is some evidence that aggressive management of serum calcium and parathyroid levels:
- Should undergo an urgent parathyroidectomy:
- Care should be taken in wound care management:
- Because aggressive debridement can lead to chronic nonhealing wounds:
- Since wound healing is very poor in these patients
- Because aggressive debridement can lead to chronic nonhealing wounds:
- Is a rare vascular disorder:
- Uremic pruritus:
- Is characterized by severe itching:
- That is thought to result from increased deposition of calcium salt in the dermis:
- Without the visible lesions of calciphylaxis
- That is thought to result from increased deposition of calcium salt in the dermis:
- Parathyroidectomy:
- Seems to alleviate these symptoms and halts progression to the more serious skin and vascular complications seen with calciphylaxis
- Is characterized by severe itching:
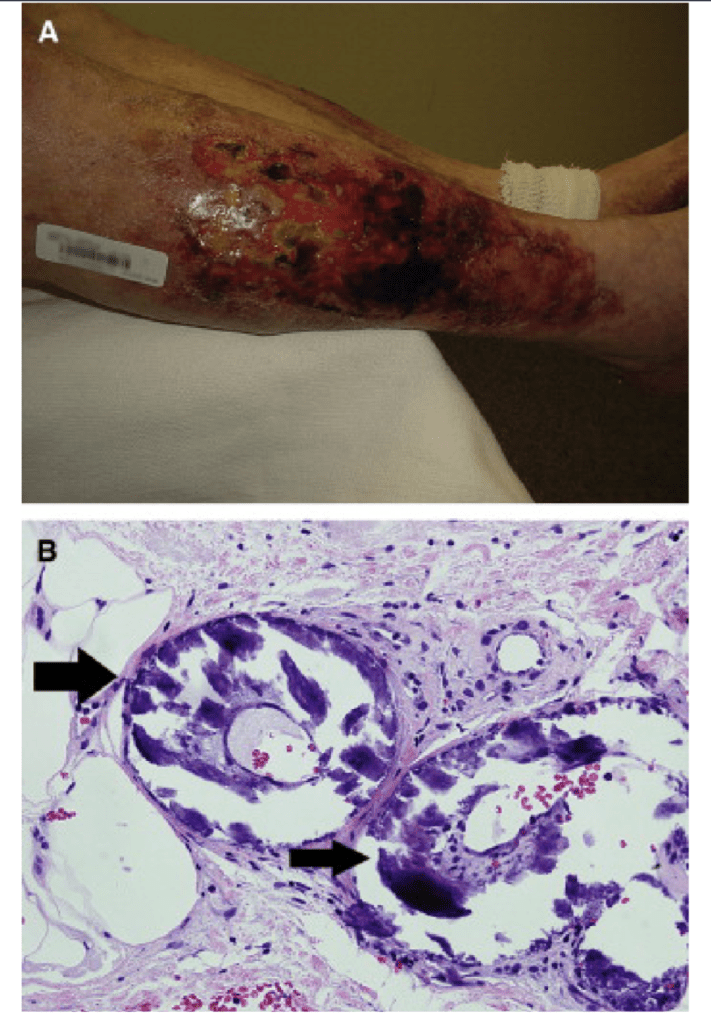
erosions with islands of intervening granulation tissue and areas of eschar. The surrounding skin was
violaceous and very tender to palpation (b). Characteristic histologic findings in calciphylaxis.
Photomicrograph (original magnification × 400) showing three blood vessels with surrounding
mineralization, indicated by arrows.

#Arrangoiz #ParathyroidSurgeon #ParathyroidExpert #EndocrineSurgery #HeadandNeckSurgeon #MSMC #Miami #MountSinaiMedicalCenter #Mexico #Teacher #Surgeon
