- Calcium:
- Is the most abundant cation in human beings and has several crucial functions
- Approximetely 900 mg
- Extracellular calcium levels:
- Are 10,000-fold higher than intracellular levels:
- Both are tightly controlled
- Are 10,000-fold higher than intracellular levels:
- Extracellular calcium:
- Is important for excitation-contraction coupling in muscle tissues, synaptic transmission in the nervous system, coagulation cascade , and secretion of other hormones
- Intracellular calcium:
- Is an important second messenger regulating cell division, motility, membrane trafficking, and secretion
- Calcium:
- Is absorbed from the small intestine:
- In its inorganic form
- Is absorbed from the small intestine:
- Calcium fluxes in the steady state are depicted in Figure
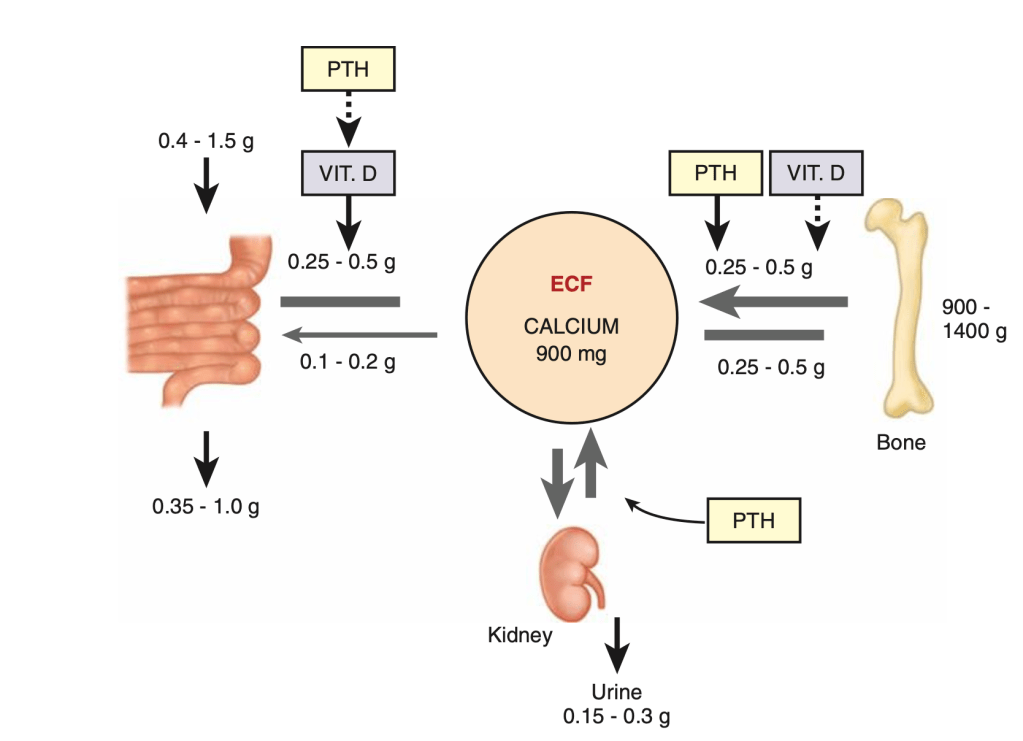
- Extracellular calcium (900 mg):
- Accounts for only 1% of the body’s calcium stores:
- The majority of which is sequestered in the skeletal system
- Approximately 50% of the serum calcium is in the ionized form:
- Which is the active component
- The remainder is bound to albumin (40%) and organic anions such as phosphate and citrate (10%)
- The total serum calcium levels range from:
- 8.5 to 10.5 mg/dL (2.1 to 2.6 mmol/L)
- Ionized calcium levels range from:
- 4.4 to 5.2 mg/dL (1.1 to 1.3 mmol/L)
- Both concentrations are tightly regulated
- Accounts for only 1% of the body’s calcium stores:
- The total serum calcium level:
- Must always be considered in its relationship to plasma protein levels:
- Especially serum albumin:
- For each gram per deciliter of alteration of serum albumin above or below 4.0 mg/dL:
- There is a 0.8 mg/dL increase or decrease in protein-bound calcium and, thus, in total serum calcium levels
- For each gram per deciliter of alteration of serum albumin above or below 4.0 mg/dL:
- Especially serum albumin:
- Must always be considered in its relationship to plasma protein levels:
- Total and, particularly, ionized calcium levels:
- Are influenced by various hormone systems
- Parathyroid Hormone
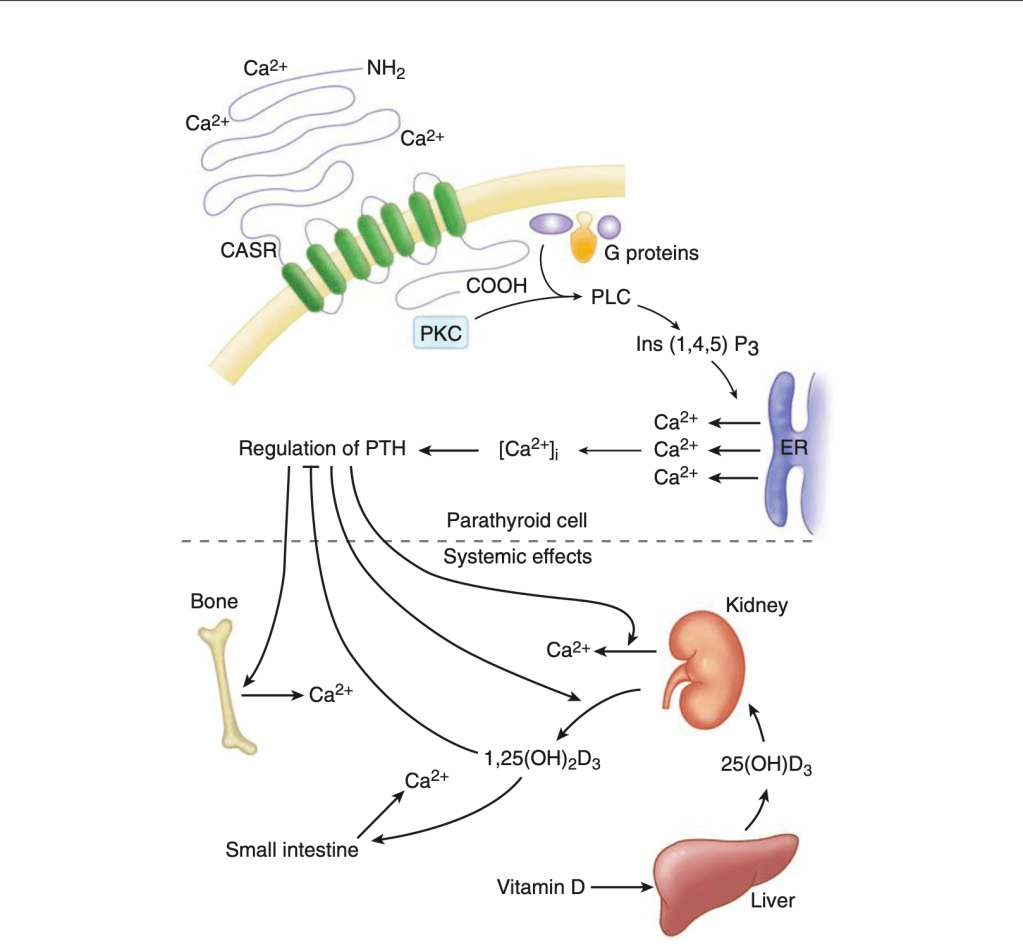
- The parathyroid cells rely on a G-protein–coupled membrane receptor:
- Designated the calcium-sensing receptor (CASR):
- To regulate PTH secretion By sensing extracellular calcium levels (Figure)
- Designated the calcium-sensing receptor (CASR):
- The parathyroid cells rely on a G-protein–coupled membrane receptor:
- PTH secretion:
- Also is stimulated by:
- Low levels of 1,25-dihydroxy vitamin D
- Catecholamines
- Hypomagnesemia
- Also is stimulated by:
- The PTH gene is located on chromosome 11
- PTH:
- Is synthesized in the parathyroid gland as a precursor hormone preproPTH:
- Which is cleaved first to pro-PTH and then to the final 84-amino-acid PTH
- Secreted PTH:
- Has a half-life of 2 to 4 minutes
- In the liver:
- PTH is metabolized into the active N-terminal component and the relatively inactive C-terminal fraction:
- The C-terminal component is excreted by the kidneys and accumulates in chronic renal failure
- PTH is metabolized into the active N-terminal component and the relatively inactive C-terminal fraction:
- Is synthesized in the parathyroid gland as a precursor hormone preproPTH:
- PTH functions to regulate calcium levels:
- Via its actions on three target organs:
- The bone, kidney, and gut
- Via its actions on three target organs:
- PTH:
- Increases the resorption of bone:
- By stimulating osteoclasts and promotes the release of calcium and phosphate into the circulation
- At the kidney, calcium is primarily absorbed in concert with sodium in the proximal convoluted tubule:
- But fine adjustments occur more distally:
- PTH acts to limit calcium excretion at the distal convoluted tubule:
- Via an active transport mechanism
- PTH acts to limit calcium excretion at the distal convoluted tubule:
- PTH also inhibits phosphate reabsorption (at the proximal convoluted tubule) and bicarbonate reabsorption
- It also inhibits the Na+ / H+ antiporter:
- Which results in a mild metabolic acidosis in hyperparathyroid states
- PTH and hypophosphatemia:
- Also enhance 1-hydroxylation of 25-hydroxyvitamin D:
- Which is responsible for its indirect effect of increasing intestinal calcium absorption
- Also enhance 1-hydroxylation of 25-hydroxyvitamin D:
- But fine adjustments occur more distally:
- Increases the resorption of bone:
- Calcitonin:
- Calcitonin is produced by thyroid C cells (parafollicular cells)
- Functions as an antihypercalcemic hormone:
- By inhibiting osteoclast-mediated bone resorption
- Calcitonin production is stimulated b:
- Calcium and pentagastrin and also by catecholamines, cholecystokinin, and glucagon
- When administered intravenously to experimental animals, it produces hypocalcemia
- At the kidney, calcitonin increases phosphate excretion by inhibiting its reabsorption
- Calcitonin plays a minimal, if any, role in the regulation of calcium levels in humans:
- However, it is very useful as a marker of MTC and in treating acute hypercalcemic crisis
- Vitamin D
- Vitamin D refers to vitamin D2 and vitamin D3:
- Both of which are produced by photolysis of naturally occurring sterol precursors
- Vitamin D2 is available commercially in pharmaeutical preparations
- Vitamin D3 is the most important physiologic compound:
- It is produced from 7-dehydrocholesterol:
- Which is found in the skin
- It is produced from 7-dehydrocholesterol:
- Vitamin D is metabolized in the liver to its primary circulating form:
- 25-hydroxyvitamin D
- Further hydroxylation in the kidney results in:
- 1,25-dihydroxy vitamin D:
- Which is the most metabolically active form of vitamin D
- 1,25-dihydroxy vitamin D:
- Vitamin D stimulates the absorption of calcium and phosphate from the gut and the resorption of calcium from the bone
- Vitamin D refers to vitamin D2 and vitamin D3:

