- The presence of clinically or microscopically detectable locoregional non-nodal disease can be broadly categorized into three groups:
- Satellites
- In-transit metastasis
- Microsatellite disease
- Satellite / in-transit patterns of recurrence:
- Are relatively unique to melanoma:
- They can occur in 3% to 10% of melanoma cases
- Although the molecular determinants and pathophysiology of in-transit disease are not fully understood:
- They are likely an intralymphatic manifestation of melanoma metastases
- Independent predictors of in-transit recurrence among patients who underwent sentinel node biopsy include:
- Age older than 50 years
- Lower-extremity primary tumor
- Increasing tumor thickness
- Ulceration
- Nodal involvement
- Are relatively unique to melanoma:
- Regional nodal metastases:
- Can occur in about two-thirds of patients with in-transit disease:
- If present, are associated with lower survival rates
- Can occur in about two-thirds of patients with in-transit disease:
- Reported predictors of distant metastasis among patients with in-transit recurrence include:
- Positive SLN status
- In-transit tumor size of at least 2 cm
- Disease-free interval before in-transit recurrence of less than 12 months
- Approach to Treatment:
- The treatment landscape for patients with locoregional non-nodal disease continues to evolve:
- It warrants a multidisciplinary team approach
- Treatment options include:
- Surgery:
- Particularly for patients with limited, resectable disease
- If surgery is performed:
- It is recommended that clear histologic margins be obtained as there is no clinical trial-informed data to support wider excision margins
- Regional approaches
- Intralesional therapy
- Systemic therapy
- Surgery:
- The treatment landscape for patients with locoregional non-nodal disease continues to evolve:
- Systemic treatment approaches:
- Have mostly supplanted regional-directed therapy for multifocal and / or unresectable disease
- Patients with in-transit metastases confined to a limb:
- That are not amenable to standard surgical measures (e.g., patients with recurrent and / or multiple in-transit metastases and patients with large-burden in-transit disease) and have failed or are not candidates for systemic therapy:
- Pose a unique treatment challenge
- Importantly, amputation is rarely indicated
- That are not amenable to standard surgical measures (e.g., patients with recurrent and / or multiple in-transit metastases and patients with large-burden in-transit disease) and have failed or are not candidates for systemic therapy:
- Hyperthermic Isolated Limb Perfusion (HILP) and Isolated Limb Infusion (ILI):
- Although infrequently employed as a component of the current melanoma treatment landscape:
- Regional chemotherapy techniques such as isolated limb infusion (ILI) or hyperthermic isolated limb perfusion (HILP) have been employed to treat in-transit metastases
- Although infrequently employed as a component of the current melanoma treatment landscape:
- Hyperthermic isolated limb perfusion (HILP) with melphalan:
- Was initially used to treat in-transit metastases of the extremities in the mid-1950s
- With this procedure, a formal lymph node dissection is performed:
- That provides exposure to the critical vessels of interest
- Subsequently, cannulae are inserted and the extremity is placed on an extracorporeal (oxygenated) bypass circuit after a tourniquet is applied:
- Effectively isolating the limb from systemic circulation
- Melphalan has been the most employed agent for use in HILP:
- Overall response rates of 64% to 100%
- Median complete response rates of 58% have been achieved
- The median response duration in patients with a complete response:
- Generally ranges from 9 to 19 months
- Although HILP was a rational treatment option for patents with in-transit metastases:
- The technique was also complex and invasive:
- To address these challenges, the technique of minimally invasive ILI was developed
- The technique was also complex and invasive:
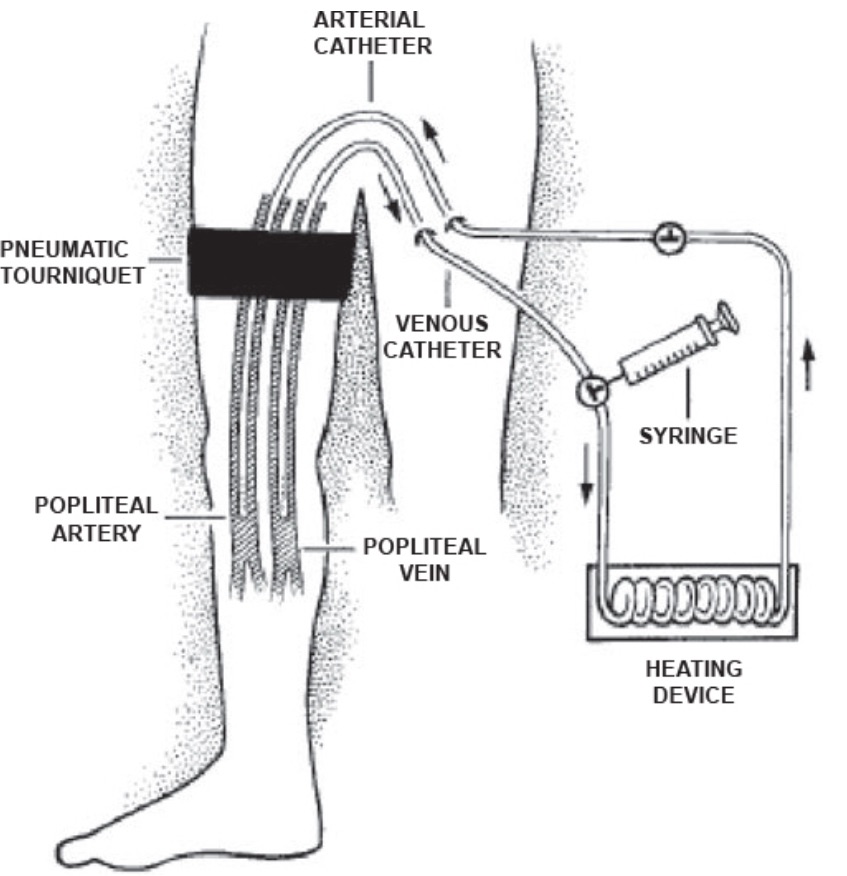
- ILI is essentially a low-flow minimally invasive isolated limb perfusion performed via percutaneously inserted catheters, and without oxygenation of the circuit (Figure):
- Using standard radiologic techniques, catheters are inserted percutaneously into the main artery and vein of the unaffected limb (or placed in the main artery and vein in the affected limb, i.e., brachial or popliteal artery and vein)
- Under general anesthesia, after a pneumatic tourniquet is inflated proximally, cytotoxic agents (generally melphalan and actinomycin-D):
- Are infused through the arterial catheter and “hand-circulated” with a syringe technique for 20 to 30 minutes:
- Progressive hypoxia occurs because, in contrast to isolated limb perfusion, no oxygenator is used
- The hypoxia and acidosis associated with ILI are therapeutically attractive because numerous cytotoxic agents, including melphalan, appear to damage tumor cells more effectively under hypoxic conditions:
- Hypoxia and acidosis have been reported to increase the cytotoxic effects of melphalan in experimental models
- Are infused through the arterial catheter and “hand-circulated” with a syringe technique for 20 to 30 minutes:
- Although the limb tissues are exposed to the cytotoxic agent for only a short period (up to 30 minutes), the procedure has been shown to yield response rates roughly like those observed after conventional HILP:
- Overall response rates of 85%
- Complete response rate of 41%
- Partial response rate of 44%
- A multi-institutional study by Beasley et al:
- Revealed a 31% complete response rate and a 33% partial response rate
- Because of the relative simplicity of the isolated infusion technique, it became a more attractive option for patients with prohibitive comorbidities or the elderly, and in general became more widely used than HILP
- Toxicity and Morbidity of HILP and ILI:
- HILP and ILI can be associated with potentially significant regional adverse effects, including:
- Myonecrosis
- Nerve injury
- Compartment syndrome
- Arterial thrombosis:
- Sometimes necessitating fasciotomy or rarely amputation
- Systemic leak of melphalan can result in additional toxicities
- Following ILI, regional adverse events appear to be similar to those reported after conventional HILP:
- With 41% of patients experiencing grade II toxic effects and 53% experiencing grade III toxic effects
- Both procedures require a high degree of technical expertise:
- If considered in the context of a multidisciplinary team-based approach, the procedure (almost exclusively ILI, as HILP is mostly of historical significance) should be performed only in centers that have experience with the technique
- Moreover, in the era of modern targeted and immunotherapies, these techniques are rarely employed
- HILP and ILI can be associated with potentially significant regional adverse effects, including:

