- The initial test recommended in the evaluation of hypothyroidism is:
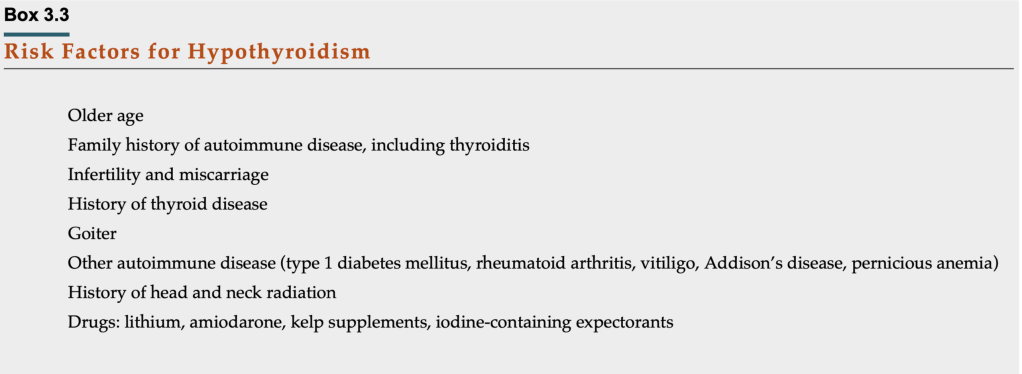
- A serum TSH concentration if the patient has any of the signs or symptoms of a hypothyroid syndrome or any of the risk factors shown in table
- The measurement of a TSH:
- Is a very sensitive and specific method to diagnose hypothyroidism
- It is almost always elevated in primary hypothyroidism:
- The TSH rise occurs before the decreases of serum T4 and / or T3 levels
- However, measurement of TSH is not a good initial test for secondary hypothyroidism:
- Thus should not be used to assess the thyroid status of a patient with known or suspected hypothalamic or pituitary disease, or in severe nonthyroidal illness
- Serum TSH is also difficult to use when thyroid hormone levels are in flux
- If thyroid hormone replacement is not initiated after thyroidectomy:
- TSH rises to > 30 mIU/L within 22 days in 95% of individuals
- An algorithm for the evaluation of hypothyroidism in an individual with signs and / or symptoms suggestive of the disease is presented in Figure
- If the serum TSH is within the normal range:
- The patient is biochemically euthyroid and no further evaluation is necessary
- If the TSH is > 10 mIU/L:
- Thyroid hormone replacement should be initiated:
- An exception is during recovery from an acute illness or in subacute thyroiditis:
- When the TSH may be transiently elevated before its normalization
- An exception is during recovery from an acute illness or in subacute thyroiditis:
- Thyroid hormone replacement should be initiated:
- If the TSH is elevated above the reference range but still < 10 mIU/L:
- It is recommended that the TSH with an estimate of free T4 and a serum TPO Ab level:
- Be repeated in 1 month
- If the TSH is elevated on repeat assessment and the free T4 (or FT4I) is decreased:
- It is recommended to start thyroid hormone replacement therapy for the treatment of overt hypothyroidism
- It is recommended that the TSH with an estimate of free T4 and a serum TPO Ab level:
- Measurement of total or free T3 levels is not indicated in the evaluation of hypothyroidism:
- Because T3 levels are maintained within the reference range:
- In mild to moderate hypothyroidism:
- Due to increased conversion of T4 to T3:
- Via the increased activity of 5′deiodinase
- Due to increased conversion of T4 to T3:
- In mild to moderate hypothyroidism:
- Because T3 levels are maintained within the reference range:

- Subclinical Hypothyroidism:
- Subclinical hypothyroidism is defined as:
- An elevated serum TSH concentration with a normal measure of free T4 (either as FT4 or FT4I)
- Of the U.S. population over age 80 years:
- Approximately 15% have a serum TSH level > 4.5 mIU/L:
- Particularly among those with serum thyroid antibody positivity
- Approximately 15% have a serum TSH level > 4.5 mIU/L:
- The optimal management of subclinical hypothyroidism has been a matter of controversy:
- Because the TSH will normalize in approximately one-third of adults over a 3- to 4-year period:
- It is important to identify those who will have persistent disease and / or those who may benefit from thyroid hormone replacement
- Because the TSH will normalize in approximately one-third of adults over a 3- to 4-year period:
- Some small, well-controlled studies:
- Have suggested a benefit toward improved well-being and a reduction in cholesterol levels:
- In subclinically hypothyroid individuals treated with thyroid hormone
- The benefit of reducing cardiovascular risk is primarily seen in middle-aged patients:
- With less improvement among older patients
- Have suggested a benefit toward improved well-being and a reduction in cholesterol levels:
- In general, the decision to treat patients with subclinical hypothyroidism:
- Depends on the presence of signs or symptoms of hypothyroidism, or the increased risk of progression to overt hypothyroidism:
- As indicated by a positive risk factor, such as:
- Sonographic evidence of thyroiditis
- Elevated serum antithyroid antibody titers
- The presence of other high-risk conditions such as:
- Cardiovascular disease
- Pregnancy
- Infertility
- As indicated by a positive risk factor, such as:
- Depends on the presence of signs or symptoms of hypothyroidism, or the increased risk of progression to overt hypothyroidism:
- If the individual is asymptomatic:
- The most conservative approach is to follow the patient clinically and repeat the TSH in 6 to 12 months or earlier as directed by signs or symptoms (Figure)
- It would also be reasonable to obtain additional data to determine the risk of progression to overt hypothyroidism, including:
- Inquiring about a family history of autoimmune thyroid disease
- Performing a thyroid ultrasound to assess for thyroiditis
- Obtaining a serum TPO Ab titer
- In one study, women with mild subclinical hypothyroidism and serum thyroid autoimmunity followed for 4 years:
- Had a 5% per year risk of developing biochemical hypothyroidism
- Subclinical hypothyroidism is defined as:
- Serum Thyroid Antibodies in Hypothyroidism:
- Measurement of serum antithyroid antibodies in the differential diagnosis of primary hypothyroidism:
- Should be interpreted in the context of the clinical findings
- TPO Ab or TgAb is positive:
- In most patients with autoimmune thyroiditis (Hashimoto’s thyroiditis)
- It is not required but confirms the diagnosis:
- Those with high titers are likely to progress more rapidly to overt hypothyroidism
- It is not required but confirms the diagnosis:
- In most patients with autoimmune thyroiditis (Hashimoto’s thyroiditis)
- Elevated serum TPO Ab and TgAb:
- Can be detected after the release of thyroid antigens:
- In patients with silent subacute thyroiditis:
- Such as postpartum thyroiditis
- In patients with silent subacute thyroiditis:
- Can be detected after the release of thyroid antigens:
- Measurement of serum antithyroid antibodies in the differential diagnosis of primary hypothyroidism:
- Thyroid Imaging in Hypothyroidism:
- Thyroid ultrasound in Hashimoto’s demonstrates:
- A characteristic irregular texture and is often associated with diffuse enlargement
- Blood flow, as assessed by Doppler:
- Is reduced in subacute thyroiditis:
- But it is difficult to distinguish reduced flow from normal
- Is reduced in subacute thyroiditis:
- Radionuclide imaging of the thyroid:
- Is almost never helpful for the diagnosis of hypothyroidism
- Thus thyroid ultrasound and / or radionuclide imaging:
- Should be performed only to evaluate suspicious structural abnormalities:
- Such as a palpable thyroid nodule in the hypothyroid patient
- Should be performed only to evaluate suspicious structural abnormalities:
- Although controversial, there is an epidemiologic association of:
- Concurrently elevated serum TSH concentrations in thyroiditis with an increased risk of thyroid malignancy
- It has been suggested that clinicians use sonography to evaluate patients with thyroiditis, Hashimoto’s thyroiditis, and Graves’ disease:
- To detect thyroid nodules:
- Which would then require biopsy based on ultrasound features
- To detect thyroid nodules:
- Thyroid ultrasound in Hashimoto’s demonstrates:
- Treatment of Hypothyroidism:
- Hypothyroidism is treated with thyroid hormone replacement:
- Usually in the form of oral T4 (levothyroxine)
- In individuals with little or no endogenous thyroid hormone production:
- The usual requirement is 1.6 mcg/kg/day
- Because 80% of circulating T3 is derived from T4:
- T4 monotherapy is adequate in most patients for thyroid hormone replacement
- Some patients, however, have persistent symptoms of hypothyroidism while on biochemically adequate levothyroxine replacement and prefer the use of T4 / T3 combined products:
- Such as desiccated thyroid
- The American Thyroid Association guidelines;
- State that there is a lack of high-quality controlled long-term outcome data:
- To routinely support the use of desiccated thyroid extract, combination synthetic T4 / T3, or T3 monotherapy:
- Over levothyroxine therapy
- To routinely support the use of desiccated thyroid extract, combination synthetic T4 / T3, or T3 monotherapy:
- State that there is a lack of high-quality controlled long-term outcome data:
- Hypothyroidism is treated with thyroid hormone replacement:
- In patients with primary hypothyroidism:
- Levothyroxine dose adjustments should be done based on a serum TSH measured 4 to 6 weeks after initiating the medication:
- Due to the long half-life of levothyroxine, which is 7 to 10 days
- The goal of treatment is a serum TSH level around the middle of the normal range:
- For otherwise healthy individuals with primary hypothyroidism
- And to suppressed TSH or a TSH level at the low end of the normal range is targeted for most patients with differentiated thyroid cancer
- Levothyroxine dose adjustments should be done based on a serum TSH measured 4 to 6 weeks after initiating the medication:

