- General:
- For groin dissection the patient is placed in a slight frog-leg position with hip externally rotated and the knee partially flexed
- Incision:
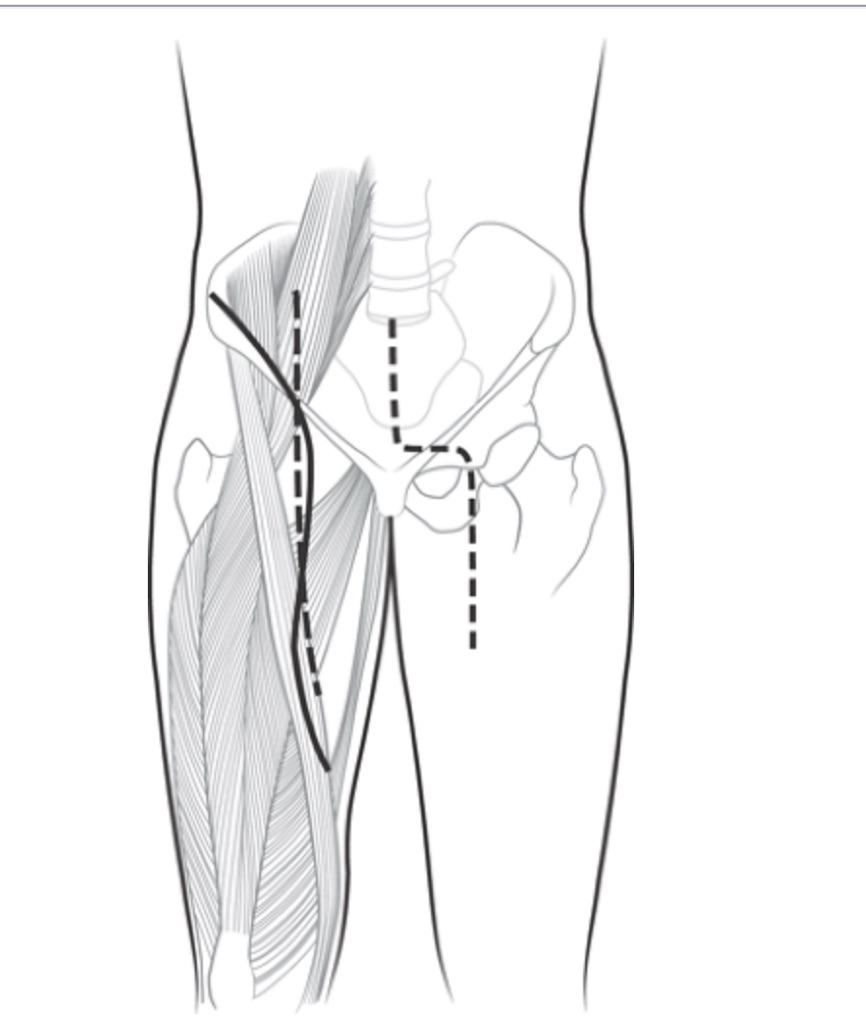
- A lazy-S incision is made from superomedial to the anterior superior iliac spine, vertically down to the inguinal crease:
- Obliquely across the crease, and then vertically down to the apex of the femoral triangle (Figure)
- Previous SLNB incisions and underlying cavities:
- Should be excised en bloc with the specimen
- A lazy-S incision is made from superomedial to the anterior superior iliac spine, vertically down to the inguinal crease:
- Skin Flaps:
- The limits of the skin flaps are:
- Medially:
- To the pubic tubercle and the midbody of the adductor magnus muscle
- Laterally:
- To the lateral edge of the sartorius muscle
- Superiorly:
- To approximately 5 cm above the inguinal ligament
- Inferiorly:
- To the apex of the femoral triangle
- Medially:
- The limits of the skin flaps are:
- Lymph Node Dissection:
- Dissection is carried down to the:
- Muscular fascia superiorly
- All fatty, node-bearing tissue is swept down to the inguinal ligament and off the external oblique fascia
- Medially, the spermatic cord or round ligament is exposed, and nodal tissue is swept laterally
- Nodal tissue is swept off the adductor fascia to the femoral vein
- At the apex of the femoral triangle, the saphenous vein is identified:
- If the saphenous vein can be preserved:
- Nodal tissue is removed from the vessel circumferentially; otherwise, it is sacrificed
- If the saphenous vein can be preserved:
- Laterally, nodal tissue is dissected off the sartorius muscle and the femoral nerve
- With dissection in the plane of the femoral vessels:
- The nodal tissue is elevated up to the level of the fossa ovalis:
- Where the saphenous vein is suture-ligated at the saphenofemoral junction if it is sacrificed
- The specimen is dissected to the inguinal ligament:
- Although excision of Cloquet node (the lowest iliac node), accompanied by intraoperative frozen-section examination, has historically sometimes been employed to inform concomitant iliac-obturator node dissection in patients without clinically apparent or suspicious deep groin metastasis, this approach is uncommonly employed currently
- The nodal tissue is elevated up to the level of the fossa ovalis:
- Dissection is carried down to the:
- Sartorius Muscle Transposition:
- If the sartorius muscle is to be transposed:
- It is divided at its origin on the anterior superior iliac spine
- The lateral femoral cutaneous nerve:
- Is preserved if possible
- The proximal neurovascular bundles going to the sartorius muscle:
- Are divided to facilitate transposition, with care to preserve others to the maximal extent possible to ensure a vascularized pedicle
- The rotated muscle is placed over the femoral vessels:
- Its is tacked to the inguinal ligament, fascia of the adductor, and vastus muscle groups
- If the sartorius muscle is to be transposed:
- Wound Closure:
- The skin edges are examined for viability and trimmed back to healthy skin, if necessary:
- Intravenous administration of fluorescein followed by examination using a Wood lamp:
- May be used to identify poorly perfused skin edges
- Intravenous administration of fluorescein followed by examination using a Wood lamp:
- Two closed-suction drains are generally placed through separate small incisions superiorly:
- One is laid medially, and the other is laid laterally within the operative wound
- The wound is closed with interrupted # 3-0 undyed absorbable sutures in the dermis and followed by skin staples or a running # 4-0 subcuticular suture
- In some patients, interrupted nylon sutures are used overlying the area of skin crease
- The skin edges are examined for viability and trimmed back to healthy skin, if necessary:
- Postoperative Management:
- The patient begins ambulating the day following surgery
- A custom-fit elastic stocking may be used during the day for 6 months
- After this period, the stocking may be discontinued if no leg swelling occurs
- Suction drainage is continued until output is less than 20 mL to 30 mL per day for 2 consecutive days
- By approximately 4 weeks, the suction catheters are removed, regardless of the amount of drainage, to mitigate risk of infection

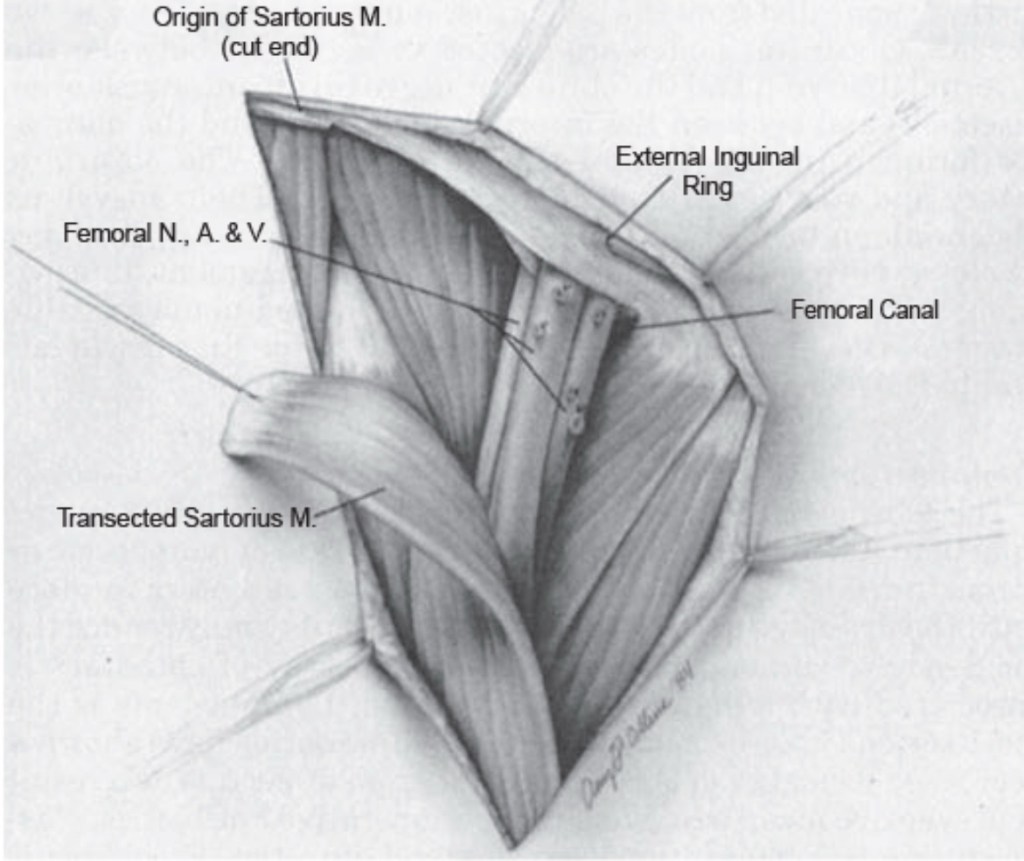
A: The borders of the femoral triangle are the inguinal ligament superiorly, the sartorius laterally, and the adductor longus medially.
B: The lymphatic contents removed during a superficial inguinal lymphadenectomy include the lymphatic contents of the femoral triangle as well as nodal tissue that lies superficial to the external oblique superior to the inguinal ligament.
C: The lazy-S incision used for an inguinal lymphadenectomy.
D: The anatomy visualized during an inguinal lymphadenectomy. (From Balch CM, Milton GW, Shaw HM, et al., eds. Cutaneous Melanoma. Lippincott; 1985.)

B: The iliac-obturator nodes include those distal to the common iliac bifurcation, and around the external and internal iliac vessels, and the obturator nodes. Obturator nodes should be excised as part of an iliac-obturator nodal dissection. (From Balch CM, Milton GW, Shaw HM, et al., eds. Cutaneous Melanoma. Lippincott; 1985.)