- The Multicenter Selective Lymphadenectomy Trial-II (MSLT-II):
- Sought to answer whether CLND was necessary following a positive SLN:
- By randomizing patients with at least one positive SLN to nodal observation (with nodal basin ultrasound, termed active surveillance) or immediate CLND after a positive SLN
- Overall, the trial accrued > 1,900 patients and at a median follow-up of 43 months, in the per-protocol analysis:
- The 3-year melanoma-specific survival (primary endpoint):
- Was similar in both the CLND group and the observation group
- Disease control in the regional nodes at 3 years:
- Was also increased in the dissection group compared to the observation group:
- 92% vs. 77%; P < .001
- Was also increased in the dissection group compared to the observation group:
- Nonsentinel node metastases:
- Identified in 11.5% of the patients in the dissection group were a strong and independent predictor of recurrence (hazard ratio, 1.78; P = .005)
- The 3-year melanoma-specific survival (primary endpoint):
- Taken together, these initial data support that immediate CLND increased regional disease control and provided prognostic information:
- But did not increase MSS in these patients with SLN metastases
- Sought to answer whether CLND was necessary following a positive SLN:
- In the German multicenter, randomized, phase III DeCOG-SLT clinical trial:
- 483 patients with a positive SLNB:
- Were randomly assigned to immediate surgery (i.e., CLND following a positive SLNB) or to regional node observation
- Of note, 66% of patients had an SLN metastasis of 1 mm or less
- At a median follow-up of 72 months, among 483 included:
- The authors found that there was no significant difference in their primary endpoint of 5-year distant metastasis-free survival:
- 67.6% versus 64.9% for the observation versus immediate complete dissection groups, respectively:
- HR 1.08, 95% CI 0.83 to 1.39
- 67.6% versus 64.9% for the observation versus immediate complete dissection groups, respectively:
- The authors found that there was no significant difference in their primary endpoint of 5-year distant metastasis-free survival:
- Furthermore, there were no significant differences in RFS and OS
- Of note, the study did not reach its target accrual of 556 patients:
- Thus reducing the power of the study
- 483 patients with a positive SLNB:
- Taken together, these trials have contributed to a significant paradigm shift in clinical practice for the patient with a positive SLN:
- As two clinical trials demonstrated that CLND provided no recurrence free survival (RFS) or OS benefit in melanoma patients with a positive sentinel node:
- The vast majority of melanoma surgical oncologists have integrated nodal observation (with active surveillance) rather than CLND as a preferred strategy into their practice
- While CLND is still considered an option for these patients according to national consensus melanoma guidelines:
- In the setting of patient preference related to availability to be surveilled, when adjuvant therapy cannot be considered, particularly in the setting of high-risk disease with increased associated risk of non-SLN involvement:
- These situations are in clinical practice rather infrequent
- In the setting of patient preference related to availability to be surveilled, when adjuvant therapy cannot be considered, particularly in the setting of high-risk disease with increased associated risk of non-SLN involvement:
- With this change in practice, new questions have arisen, including the optimal screening algorithm for patients undergoing observation with a positive sentinel node
- As two clinical trials demonstrated that CLND provided no recurrence free survival (RFS) or OS benefit in melanoma patients with a positive sentinel node:
- In the post MSLT-II era:
- CLND is generally recommended in the context of multidisciplinary team-based care for regional recurrence discovered during active surveillance / nodal observation post SLN biopsy
- Historical Context:
- CLND was traditionally recommended for all patients with a positive sentinel lymph node (SLN) to:
- Remove additional metastatic disease
- Improve regional control
- Potentially improve survival
- CLND was traditionally recommended for all patients with a positive sentinel lymph node (SLN) to:
- Paradigm Shift:
- Key Randomized Trials:
- MSLT-II (Multicenter Selective Lymphadenectomy Trial II)
Compared CLND vs observation with ultrasound in SLN-positive patients- Findings:
- No difference in melanoma-specific survival (MSS)
- Improved regional disease control with CLND (92% vs 77%)
- Increased surgical morbidity (e.g., lymphedema) in CLND group
- Reference:
- Faries MB, et al. N Engl J Med. 2017;376(23):2211–2222.
- Findings:
- DeCOG-SLT Trial:
- German study with similar design and findings
- Conclusion:
- CLND did not improve survival in SLN-positive patients
- Reference:
- Leiter U, et al. Lancet Oncol. 2016;17(6):757–767.
- MSLT-II (Multicenter Selective Lymphadenectomy Trial II)
- Key Randomized Trials:
- Current Guidelines:
- Routine CLND is no longer recommended for all SLN-positive patients
- Patients should undergo:
- Active surveillance with high-resolution ultrasound
- Consideration of adjuvant systemic therapy:
- Particularly if high-risk
- References:
- NCCN Guidelines: Melanoma, Version 2.2024
- ASCO/SSO Clinical Practice Guidelines, Wong SL, et al. J Clin Oncol. 2018;36(4):399–413.
- Indications for Selective CLND:
- CLND may still be considered in select high-risk cases:
- Clinically palpable disease or radiographic nodal enlargement
- Extensive SLN involvement:
- > 3 mm tumor burden
- Extracapsular extension
- Nodal recurrence during observation
- CLND may still be considered in select high-risk cases:
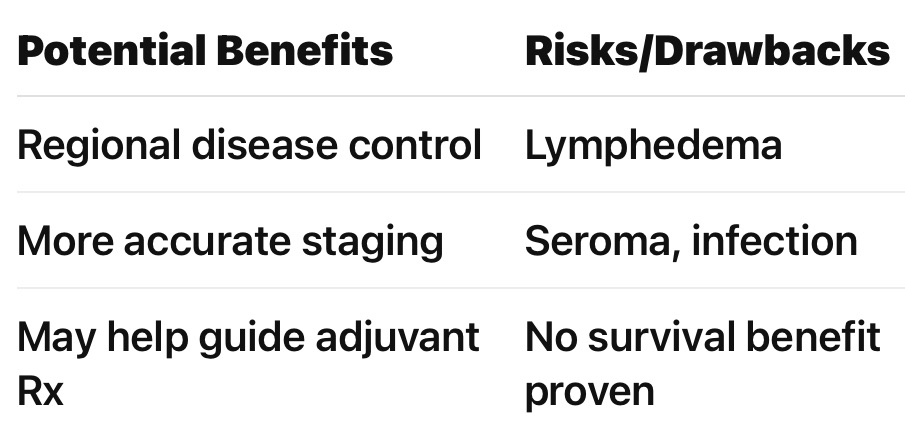
Benefits and Risks of CLND.
- Prognostic Implications:
- Presence of additional non-sentinel node (NSLN) metastases worsens prognosis
- SLN tumor burden and other risk factors help stratify who may harbor additional disease
- Conclusion:
- Routine CLND is no longer standard for SLN-positive melanoma patients following the MSLT-II and DeCOG-SLT trials
- Management now emphasizes non-invasive surveillance and adjuvant systemic therapy
- Selective CLND may still play a role in carefully chosen high-risk patients

