- Regional lymph nodes:
- Are the most common site of melanoma metastasis
- Lymph node involvement is categorized as:
- Clinically occult:
- Detected by sentinel lymph node mapping (SLNM) and sentinel lymph biopsy (SLNB)
- Clinically detected:
- Palpable and / or radiographically detected nodes
- Clinically occult:
- Fine-needle aspiration or core biopsy:
- Can usually yield a diagnosis in patients who develop clinically enlarged regional nodes
- Incisional or excisional biopsy:
- Is rarely indicated for diagnostic purposes
- Intraoperative Lymphatic Mapping and Sentinel Lymph Node Biopsy:
- Beginning in the 1990s after its introduction by Morton and colleagues:
- Several investigators proposed intraoperative lymphatic mapping and SLNB as a minimally invasive procedure for identifying approximately 15% to 20% of patients offered the procedure who harbor occult microscopic disease
- This approach is sometimes termed selective lymphadenectomy
- From a historical standpoint as initially proposed by Morton:
- The SLNB approach facilitates identification of patients for whom completion lymph node dissection would be recommended
- Several studies have demonstrated that the SLNs are the first nodes to contain metastases, if metastases are present, and thus the pathologic status of the SLNs reflects that of the entire regional nodal basin
- If the SLN lacks metastasis, the rest of the regional lymph nodes are unlikely to contain disease, and a completion lymphadenectomy (CLND) would therefore be unnecessary
- Multiple studies have demonstrated that the immediate false-negative rate for SLNB is less than 5%
- Other studies have confirmed the validity of the SLN concept and the accuracy of SLNB as a staging procedure
- It is imperative, however, that the surgeon employing SLNB has adequate pathology and nuclear medicine support
- Beginning in the 1990s after its introduction by Morton and colleagues:
- Sentinel Lymph Node Biopsy Technique:
- It is strongly preferred that lymphatic mapping and SLNB be performed at the time of wide excision of the primary melanoma
- If a wide excision has already been performed, SLNB can still generally be performed with equivalent accuracy:
- However, prior extensive reconstruction of the primary melanoma wide excision site (e.g., by extensive rotational flap reconstruction) that alters lymphatic pathways in the region:
- May significantly reduce the accuracy of this technique if performed after wide excision in such patients
- However, prior extensive reconstruction of the primary melanoma wide excision site (e.g., by extensive rotational flap reconstruction) that alters lymphatic pathways in the region:
- Since the introduction of lymphatic mapping and SLNB, the technique has undergone several refinements that have resulted in improved detection of SLNs:
- Use of a vital blue dye to identify SLNs has been part of the technique since its introduction:
- I typically use isosulfan blue 1% or Lymphazurin at our institution
- If a patient is noted to have a significant history of allergic reactions:
- You may substitute methylene blue and anecdotally note overall similar results and a favorable side effect profile
- Some surgeons prefer to give prophylaxis to prevent allergic reactions:
- Using a cocktail of I.V. diphenhydramine, I.V. hydrocortisone, and I.V. famotidine administered prior to injection of isosulfan blue
- Use of a vital blue dye to identify SLNs has been part of the technique since its introduction:
- The blue dye is injected intradermally:
- Around the residual intact tumor or biopsy site:
- It is taken up by the lymphatic system and carried via afferent lymphatics to the SLN(s)
- The draining nodal basin is explored, and the afferent lymphatic channels and first draining lymph nodes (the SLNs) are identified by the uptake of the blue dye
- Around the residual intact tumor or biopsy site:
- With the use of blue dye alone, an approach utilized mostly in the early 1990s:
- An SLN was identified in approximately 85% of cases:
- Although this initial approach was promising, 15% of patients were unable to benefit from the procedure because no SLN was identified
- An SLN was identified in approximately 85% of cases:
- Subsequently, additional techniques were incorporated that have significantly improved SLN localization:
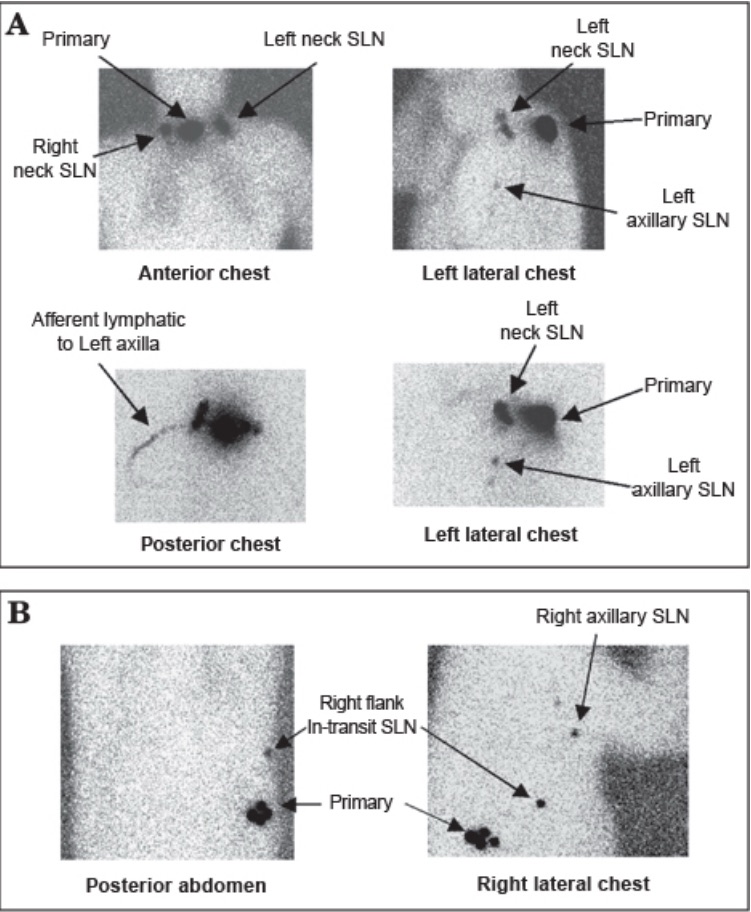
- Preoperative lymphoscintigraphy
- Intradermal injection of technetium-99 (99Tc)-labeled sulfur colloid accompanied by intraoperative use of a handheld gamma probe
- Preoperative lymphoscintigraphy using 99Tc-labeled sulfur colloid:
- Facilitates the identification of patients with multiple draining nodal basins and patients with lymphatic drainage to SLNs located outside standard nodal basins, including:
- Epitrochlear, popliteal, and ectopic /interval / in-transit sites
- Facilitates the identification of patients with multiple draining nodal basins and patients with lymphatic drainage to SLNs located outside standard nodal basins, including:
- In 2013, Tc 99m tilmanocept (Lymphoseek):
- Was approved by the FDA as a receptor-targeted lymphatic mapping agent:
- Whose mechanism of action is to bind to mannose receptors on lymphatic tissue
- It accumulates in lymphatic tissue within minutes and facilitates localization of SLNs:
- It can be used in place of 99Tc-labeled sulfur colloid for both lymphoscintigraphic imaging as well as for intraoperative management
- Was approved by the FDA as a receptor-targeted lymphatic mapping agent:
- In patients with melanomas that drain to multiple regional nodal basins:
- The histologic status of one draining basin does not predict the status of other basins:
- Therefore, it is particularly important to identify and assess all at-risk regional nodal basins to properly stage the patient
- The histologic status of one draining basin does not predict the status of other basins:
- An advance from traditional nuclear imaging is the use of single-photon emission computed tomography (SPECT) imaging merged with CT:
- SPECT / CT facilitates localization of SLNs by overlaying radiotracer uptake activity onto the noncontrast CT image and is particularly helpful in the head and neck region:
- In one study, the surgical approach was revised because of SPECT / CT imaging in up to 30% of cases
- SPECT / CT facilitates localization of SLNs by overlaying radiotracer uptake activity onto the noncontrast CT image and is particularly helpful in the head and neck region:

- Perhaps the most important development in the SLNB technique:
- Has been the introduction of intraoperative lymphatic mapping:
- Using a handheld gamma probe
- In this approach, 0.5-mCi 99Tc-labeled sulfur colloid, or Lymphoseek is injected intradermally prior to surgery, either in nuclear medicine prior to arrival in the operating room (sometimes in concert with preoperative lymphoscintigraphy) or after induction of general anesthesia
- During surgery, a handheld gamma probe is used to transcutaneously identify SLNs to facilitate their removal
- The use of both blue dye and radiotracer increases the surgeon’s ability to identify the SLN (> 96% to 99% sensitivity) compared to the use of blue dye alone (≈ 84% sensitivity)
- Although most clinicians use a combined modality approach, some favor the single-agent strategy of radiotracer alone, and some have reported similarly excellent sensitivity compared to a combination strategy
- Has been the introduction of intraoperative lymphatic mapping:

