- Thyroid Stimulating Hormone (TSH):
- Is produced from the anterior pituitary gland:
- After stimulation by thyrotropin-releasing hormone (TRH)
- Is produced from the anterior pituitary gland:
- Thyrotropin-releasing hormone (TRH):
- Is a modified three-amino acid peptide:
- Produced by neurons of the paraventricular nucleus:
- In the hypothalamus
- Produced by neurons of the paraventricular nucleus:
- TRH signaling from the hypothalamus:
- Is achieved through a portal venous system:
- Located in the infundibulum of the pituitary stalk:
- Which allows communication to the pituitary gland
- Located in the infundibulum of the pituitary stalk:
- Is achieved through a portal venous system:
- Is a modified three-amino acid peptide:
- Both TRH and TSH gene expression:
- Are decreased by excess thyroid hormone levels:
- Via negative feedback mechanisms (Figure)
- Both the hypothalamus and pituitary:
- Have high levels of 5′deiodinases Type 2 enzyme (Dio2):
- Catalyzes the removal of the 5′ iodine from the outer ring of thyroxine (T4):
- To create the metabolically active triiodothyronine (T3)
- So T4 levels are the primary feedback:
- T4 is converted locally to T3:
- Which suppresses TRH and TSH gene expression
- T4 is converted locally to T3:
- Catalyzes the removal of the 5′ iodine from the outer ring of thyroxine (T4):
- Have high levels of 5′deiodinases Type 2 enzyme (Dio2):
- Are decreased by excess thyroid hormone levels:

High concentrations of T3 suppress TSH release, and low concentrations enhance the expression of TSH. Thyrotropin-releasing hormone (TRH) also stimulates TSH release, and its absence results in failure of the thyrotroph to release TSH, resulting in hypothyroidism. TRH is secreted by neurons in the paraventricular nuclei in the hypothalamus and reaches the anterior pituitary via the hypothalamic hypophyseal portal venous system. TSH travels through the circulatory system to stimulate the thyroid and to produce thyroid hormones T4 and T3. By negative feedback inhibition, the circulating thyroid hormones suppress the production and excretion of TRH and TSH to bring the system back into equilibrium to maintain tight control over circulating thyroid hormone levels.
- Pituitary TSH is secreted in a pulsatile manner:
- Higher levels at night and lower levels during the day:
- The inverse of the cortisol cycle
- Although pulse frequency is increased nocturnally to result in a diurnal variation of TSH concentrations:
- Levels remain within the reference range
- Generally, laboratory testing of serum TSH concentrations during daylight hours:
- Is not substantially affected by the diurnal variation of TSH secretion:
- But results outside the reference range may occur in euthyroid individuals when drawn outside of these times
- Is not substantially affected by the diurnal variation of TSH secretion:
- Higher levels at night and lower levels during the day:
- TSH stimulates the synthesis and release of thyroid hormone from the thyroid gland:
- TSH production from the anterior pituitary gland is inverse log-linearly regulated by serum thyroid hormone concentrations:
- When there are small decreases in thyroid hormone levels in circulation:
- Large increases in serum TSH stimulate thyroid hormone production by the thyroid gland
- This negative feedback loop between serum TSH and the serum-free thyroid hormones:
- Is able to maintain circulating thyroid levels within a tight range
- When there are small decreases in thyroid hormone levels in circulation:
- TSH production from the anterior pituitary gland is inverse log-linearly regulated by serum thyroid hormone concentrations:
- Serum TSH is the preferred screening test:
- In the evaluation of thyroid function in the ambulatory patient:
- Regardless of whether the patient is taking thyroid hormone replacement medication
- In the evaluation of thyroid function in the ambulatory patient:
- For the healthy patient in an ambulatory setting:
- The diagnosis of hypothyroidism or hyperthyroidism:
- May be determined with approximately 98% sensitivity and 92% specificity using serum TSH
- In addition, TSH has a narrow intraindividual variability of ± 0.5 mIU/L:
- Such that thyroid dysfunction may be present if there are significant changes in TSH values over time in an individual, even if they remain within the reference range
- In certain situations, however, such as known or suspected pituitary or hypothalamic dysfunction, recent hyperthyroidism, critical illness, starvation, use of certain medications (dopamine or high-dose glucocorticoids), interference with serum thyroid autoantibodies, and thyroid hormone resistance syndromes:
- The TSH level is inaccurate for the thyroidal status and should not be used in isolation to determine thyroid function
- In addition, the presence of interfering heterophile antibodies (antibodies against the animal-derived antibodies used in the immunometric assay):
- May rarely cause abnormally high or low TSH levels:
- These conditions should be suspected when the pattern of the TSH levels does not correlate to the clinical presentation or when the peripheral serum hormone levels do not change as expected with elevated or suppressed serum TSH concentrations
- May rarely cause abnormally high or low TSH levels:
- Serum TSH assays:
- Have evolved considerably since measurements were first described in the 1960s:
- When the functional sensitivity was between 1 and 2 mIU/L
- The commonly used second-generation TSH assays have an improved functional lower limit of 0.10 to 0.20 mIU/L:
- Which is able to differentiate between euthyroid and hyperthyroid states but does not indicate the degree of hyperthyroidism
- In contrast, a third-generation TSH assay can detect levels as low as 0.01 to 0.02 mIU/L:
- This is helpful when there is a challenging pattern of serum thyroid function tests that include an extremely suppressed TSH
- In the rare instance they are needed, fourth-generation immunochemiluminometric assays are capable of detecting TSH levels in the range of 0.01 to 0.001 mIU/L
- Have evolved considerably since measurements were first described in the 1960s:
- A serum TSH level measured in an ambulatory population that lies within the reference range:
- Is generally considered evidence of normal thyroid function and requires no additional testing
- Reference ranges for serum TSH can vary slightly from one commercial laboratory to another:
- It should be noted that normal ranges, which are based on the epidemiologic distribution of serum TSH concentrations in healthy populations:
- From which serum thyroid autoantibody positivity and iodine status (both of which can affect TSH), may be variable
- It should be noted that normal ranges, which are based on the epidemiologic distribution of serum TSH concentrations in healthy populations:
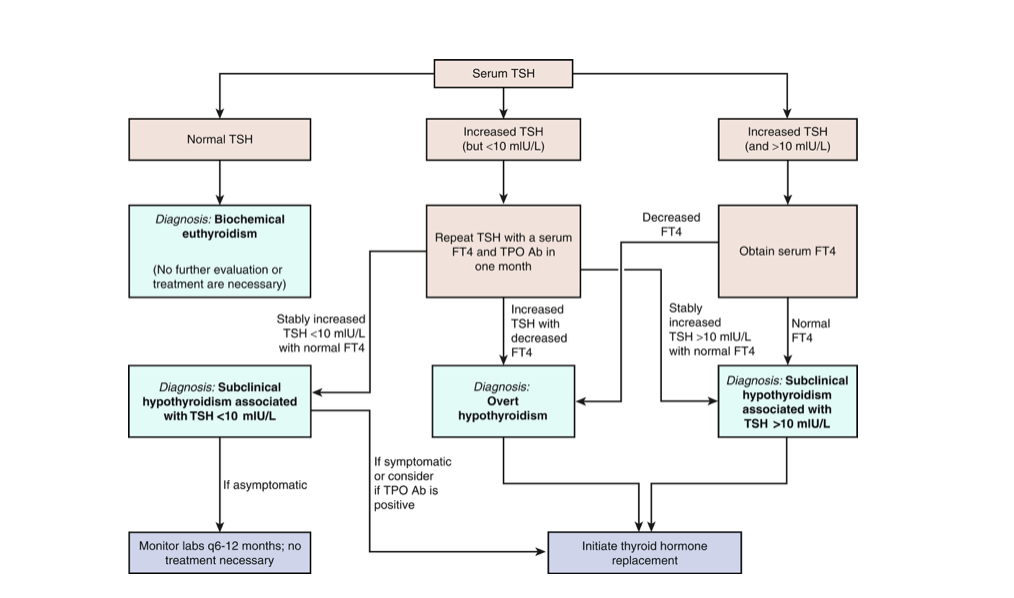
- If an abnormal screening TSH result is encountered:
- The circulating thyroid hormone levels should be assessed
- The specific pattern of tests will allow further insight into whether clinical thyroid dysfunction should be suspected
- The circulating thyroid hormone levels should be assessed