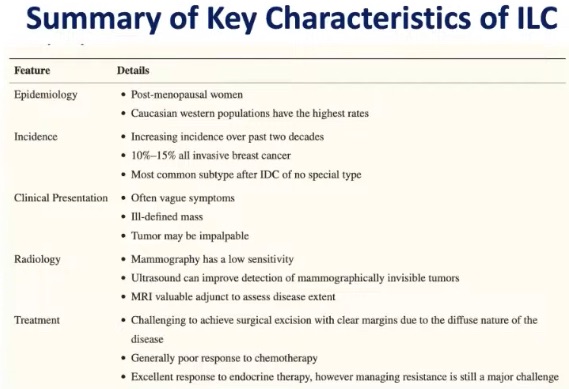
- Invasive lobular carcinoma (ILC):
- Is the second most common histologic form of breast cancer:
- Comprising 10% to 15% of invasive tumors
- Is the second most common histologic form of breast cancer:
- ILC is pathologically distinct from the much more common invasive ductal carcinoma (IDC):
- With a unique clinical biology and pathogenesis and resultant implications for diagnosis and treatment
- The mean age at diagnosis of ILC:
- Is 57 years
- Demonstrated risk factors include:
- Age at menarche
- Age at first birth
- Hormone therapy:
- Emphasizing the role of estrogen exposure in disease pathogenesis:
- Which is also observed in most IDCs:
- But shows a more pronounced association in ILC
- Which is also observed in most IDCs:
- Emphasizing the role of estrogen exposure in disease pathogenesis:
- ILC also displays an increased propensity for:
- Multifocal / multicentric presentation
- The incidence of ILC in the Western world over the past decades has corresponded to trends in the use of hormone replacement therapies:
- With a sharp increase between 1975 and
2000 and a decline between 2000 and 2004:- But now with an increasing incidence since 2005 with an unclear etiology
- With a sharp increase between 1975 and
- Hereditary ILC:
- Is rare but may be seen as a secondary tumor in families with hereditary diffuse gastric cancer syndrome:
- Caused by a germline mutation in the tumor suppressor CDH1 gene
- ILC otherwise accounts for a small minority of the breast cancers associated with known breast cancer susceptibility genes:
- Comprising less than 5% of breast cancers in patients with BRCA1 or TP53 mutations and less than 10% of breast cancers in those with BRCA2 mutations
- Is rare but may be seen as a secondary tumor in families with hereditary diffuse gastric cancer syndrome:
- Molecular characteristics of invasive lobular carcinoma (ILC):
- Classic ILC is characterized by discohesive cells that infiltrate the breast stroma in a distinctive
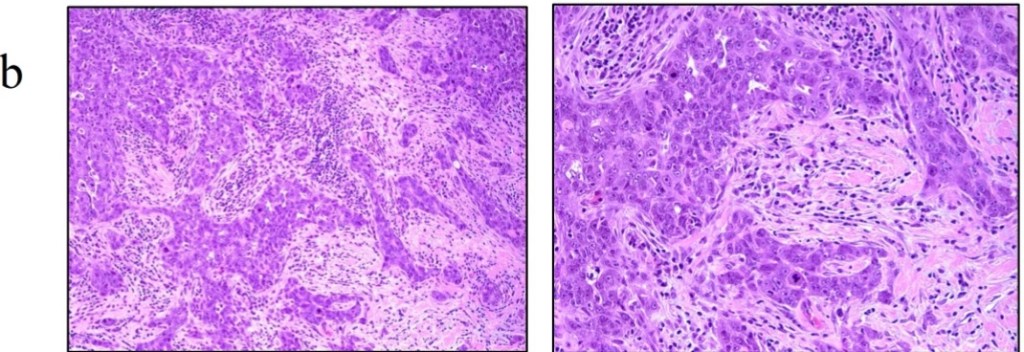
single-file pattern, with a limited host inflammatory response [Figure 1 a and b] - Several variant (nonclassic) forms of ILC have also been described:
- Distinguished by morphology:
- Dispersed, alveolar, solid, trabecular, and mixed
- Distinguished by cytology:
- Pleomorphic, apocrine, histiocytoid, signet ring, and tubulolobular
- They have inactivation of CDH1
- Frequent mutations in the PIK3CA pathways
- Gain in chromosome 1q and loss of 16q
- Majority are luminal A intrinsic subtype
- Distinguished by morphology:
- Classic ILC is characterized by discohesive cells that infiltrate the breast stroma in a distinctive
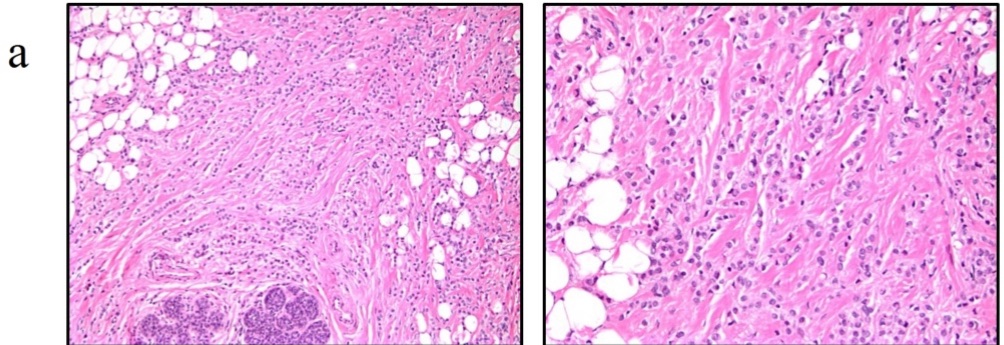
original magnification).
- Over 90% of ILCs are:
- Estrogen receptor (ER) positive
- At the level of the transcriptome:
- The majority of ILCs are classified as luminal A
- This proportion is observed to be slightly lower in more aggressive ILC variants
- The majority of ILCs are classified as luminal A
- HER-2 overexpression is rare:
- Seen in 3% to 5% of classic ILCs:
- Although it is more frequent in up to 10% of ILC variants:
- Particularly the pleomorphic subgroup, and recurrent ILCs
- Although it is more frequent in up to 10% of ILC variants:
- Seen in 3% to 5% of classic ILCs:
- The more aggressive biology of the pleomorphic subgroup renders it a unique clinical entity:
- Shown to present at a more advanced stage and more frequently metastasize
- The tumor biology of ILCs, as with all breast cancers:
- Is of focal importance in both surgical and systemic treatment, as well as long-term outcomes
- Loss of E-cadherin expression:
- Is the most consistently reported hallmark feature of ILC:
- Seen in 80% to 90% of cases
- It is believed to play an early and important role:
- In disease pathogenesis
- E-cadherin dysregulation originates from:
- Mutations in the CDH1 gene located on chromosome 16q22.1:
- Reported to occur at a frequency ranging from 30% to 80% in ILC
- Mutations in the CDH1 gene located on chromosome 16q22.1:
- E-cadherin is a calcium-dependent transmembrane protein:
- That forms a crucial component of adherens-type junctions between epithelial cells:
- The loss of which predisposes to neoplastic proliferation
- That forms a crucial component of adherens-type junctions between epithelial cells:
- However, E-cadherin positivity does not, by itself, exclude a lobular neoplasm, and not all ILCs harbor CDH1 gene mutations
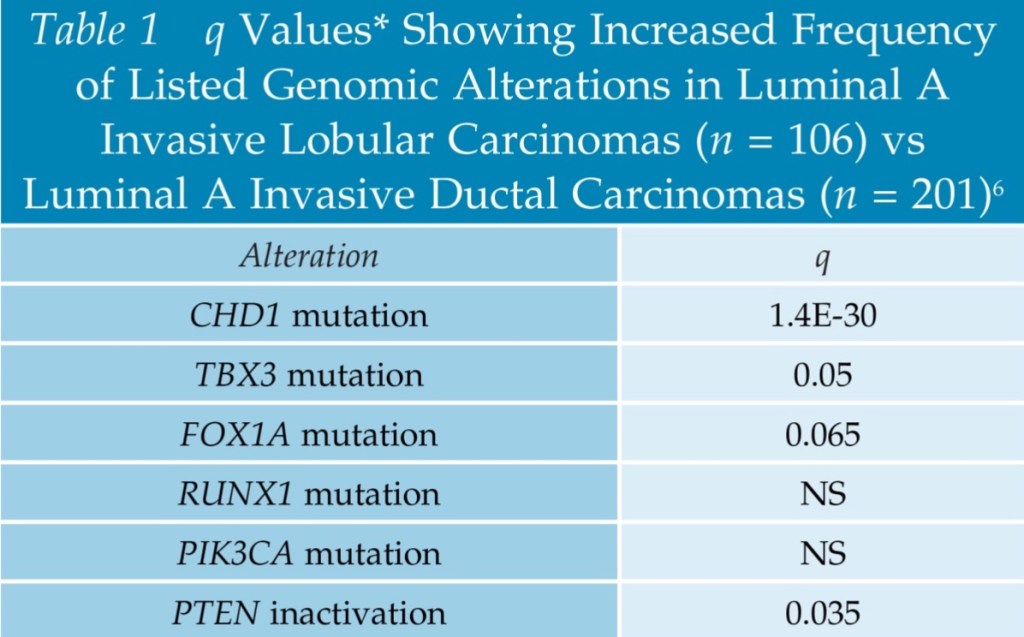
- Several other novel mutations have recently been identified as more frequent in ILC compared with IDC:
- By comprehensive molecular profiling of 817 breast tumors in The Cancer Genome Analysis (TCGA) study:
- Seen both when comparing all ILCs with IDCs and when limiting comparison with luminal A samples
- By comprehensive molecular profiling of 817 breast tumors in The Cancer Genome Analysis (TCGA) study:
- When comparing all cancers, alterations more frequently seen in ILC included:
- CDH1 (63% in ILC versus 2% in IDC)
- P1K3CA (48% versus 33%)
- FOXA1 (7% versus 2%)
- RUNX1 (10% versus 3%)
- TBX3 (9% versus 2%)
- Conversely, GATA3 mutations were enriched in:
- IDC (5% in ILC versus 13% in IDC)
- Importantly, when the analysis was limited to luminal A samples only, several alterations remained significantly more common among luminal A ILCs versus luminal A IDCs, as summarized here (Table)
- Is the most consistently reported hallmark feature of ILC: