- Axillary evaluation in DCIS:
- To do or not to do?
- As a rule NOT to do
- To do or not to do?
- The risk of underlying invasion in patients with DCIS:
- Is roughly 25% (Bundred et al, BMJ. 2013) in this era of core biopsies
- Risk of SLN metastasis in pure DCIS:
- Is 0.2% to 0.7% (Zetterfund et al; BJS. 2014; Nicholson et al, EJSO. 2015):
- Risk may rise to 9% if known micro-invasion (Meretoja et al, Ann Surg Onc. 2009)
- Is 0.2% to 0.7% (Zetterfund et al; BJS. 2014; Nicholson et al, EJSO. 2015):
- Vacuum assisted devices (VAB):
- Can lower the risk of invasion to 11% in retrospective data (Sumian et al, EJSO, 2016)
- In prospective data (Cinnamome Study):
- The upgrade was 39% (Tunon-De-Lara, Ann Surg Onco. 2015)
- Routine MRI does not improve surgical outcomes:
- Upgrade, size, or re-excision rates
- (Fancellu et al, BJS. 2015; Chou et al ECON-AGRIN E4112, Radiology. 2021; Roque et al, NPJ breast cancer. 2022)
- Upgrade, size, or re-excision rates
- Dedicated breast PET? (Grana-Lopez et l Eur J Rad. 2020; Sasada et al, EJSO. 2021):
- Up to know have not shown improve outcomes
- There are approximately 50 retrospective studies evaluating nomograms and there predictive value on the risk of finding invasion in DCIS:
- The usual risk factors are:
- Size, grade 2 and 3, comedo necrosis, mass effect, micro-invasion:
- Among “high-risk” DCIS:
- Axillary evaluation in DCIS affects treatment but not survival (Coromilas et al, Ann Surg Onc 2016)
- Among “high-risk” DCIS:
- Size, grade 2 and 3, comedo necrosis, mass effect, micro-invasion:
- The usual risk factors are:
- Axillary evaluation in DCIS increases complications and long-term morbidity (relative increase up to 6 to 8 times (Kilelea et al, Ann Surg Onc. 2018)
- SLNB can be omitted in patients with DCIS planned for breast conserving surgery (BCS):
- Detection rate at reoperation is 85.5% (GATA Study, Breast 2015)
- NO data on feasibility after oncoplastic surgery
- NO data on procedure accuracy
- DCIS is noninvasive:
- By definition, is unable to metastasize:
- However, some studies have shown that up to 15% of patients with pure DCIS have isolated tumor cells (ITCs) or micrometastasis on nodal evaluation compared to others that show a 0.2% to 0.7% risk of nodal metastasis:
- However, these small tumor deposits likely have little prognostic significance and may be cell clusters displaced by biopsy
- However, some studies have shown that up to 15% of patients with pure DCIS have isolated tumor cells (ITCs) or micrometastasis on nodal evaluation compared to others that show a 0.2% to 0.7% risk of nodal metastasis:
- In patients with DCIS detected by core biopsy:
- There is a 15% to 25% associated risk of an invasive component when excised
- Patients undergoing mastectomy for DCIS:
- Should be offered SLNB since it would not be feasible to perform following mastectomy if invasive carcinoma is subsequently identified
- ASCO consensus guidelines recommend that patients with DCIS who undergo breast-conserving operation should not routinely have SLNB:
- However, SLNB could be discussed with patients undergoing breast conservation:
- Who have a core biopsy diagnosis of DCIS and:
- A large area of DCIS on imaging (2 to 5 cm)
- High-grade DCIS
- Comedonecrosis
- When a physical examination or imaging shows a discrete mass
- These findings have been associated with an increased risk of invasive cancer, and SLNB at the time of the initial operation could avoid a second operation
- Who have a core biopsy diagnosis of DCIS and:
- However, SLNB could be discussed with patients undergoing breast conservation:
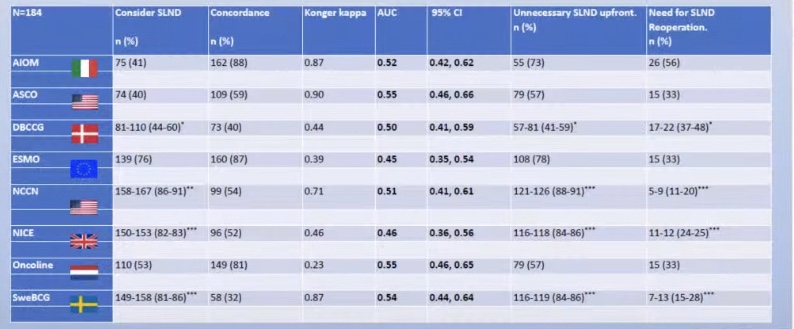
- All of the guidelines that try and help us decide when to perform of SLNB in DCIS show a predictive value of a coin toss.
- By definition, is unable to metastasize: