- Oncocytic follicular cell–derived thyroid carcinomas as a group can include many different entities:
- Oncocytic papillary thyroid carcinomas (PTC)
- Oncocytic encapsulated follicular subtype of PTC
- Oncocytic poorly differentiated carcinoma
- Oncocytic medullary thyroid carcinoma
- The term “oncocytic carcinoma of the thyroid”:
- Is used in the new World Health Organization (WHO) to refer to:
- Invasive malignant follicular cell neoplasms:
- Composed of at least 75% oncocytic cells:
- In which the nuclear features of PTC and high-grade features are absent
- Composed of at least 75% oncocytic cells:
- Invasive malignant follicular cell neoplasms:
- This term replaces Hürthle cell carcinoma:
- A misnomer given that Hürthle actually described parafollicular C cells
- Oncocytic cells:
- Have abundant granular eosinophilic cytoplasm:
- Secondary to a marked accumulation of dysfunctional mitochondria
- Have abundant granular eosinophilic cytoplasm:
- Oncocytic carcinoma of the thyroid (OCA):
- Represents the malignant counterpart of oncocytic adenoma
- Accounts for approaching 2% to 5% of differentiated thyroid carcinomas in the USA
- Can occur anywhere in the thyroid
- Usually presents as a slowly enlarging painless solitary thyroid nodule
- Thyroid ultrasound cannot distinguish between oncocytic adenoma and OCA:
- Though larger tumors have a higher rate of malignancy
- There are no known risk factors for developing OCA
- The mean age at diagnosis is approaching 60 years:
- Which is roughly 10 years later than the mean age of diagnosis for patient with follicular thyroid carcinoma
- OCA, although more common in women (with a 1.6 to 1 female-to-male ratio):
- Has a lower female-to-male ratio than is seen with follicular thyroid carcinoma
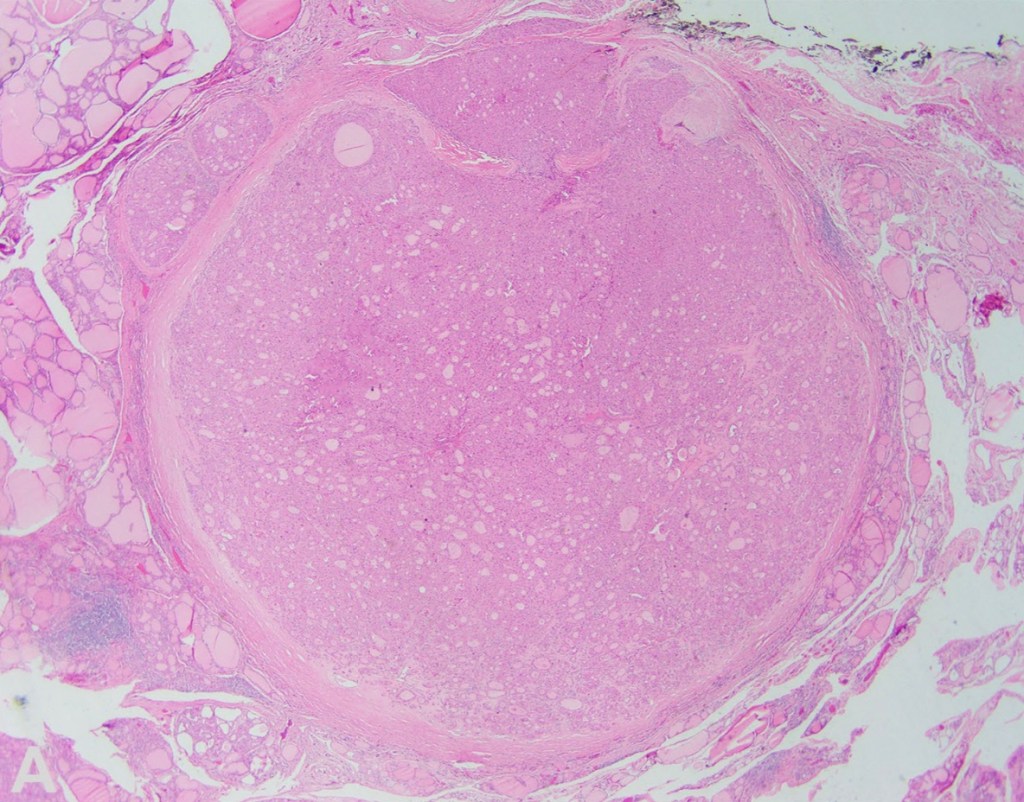
- Histologically:
- OCAs are encapsulated tumors with capsular and / or vascular invasion and at least 75% oncocytic cells (Figures)
- OCAs are subclassified into:
- Minimally invasive:
- Those with capsular invasion only
- Encapsulated angioinvasive
- Widely invasive:
- Those with gross invasion through the gland
- Minimally invasive:
- When evaluating OCA, it is important not only to document extent of invasion, but also to evaluate for progression to oncocytic poorly differentiated thyroid carcinoma:
- Thus, all tumors should be assessed for increased mitotic activity (3 or more mitoses per 10 high-power fields / ~ 2 mm2) and tumor necrosis
- OCA can metastasize to lymph nodes:
- However, some authors have shown that most of the so-called lymph nodes metastasis of OCA represent tumor plugs in veins in the neck and not lymph nodes involved by tumor
- The important clue is the almost perfect roundness of these tumor plugs compared to oval or somewhat irregular outline for nodal metastases
- OCA (like follicular thyroid carcinoma) usually spreads to distant sites via blood vessels:
- Distant metastasis at presentation are seen in 15% to 27% of patients with OCA:
- In up to 40% of tumors with extensive vascular invasion
- Distant metastasis at presentation are seen in 15% to 27% of patients with OCA:
- Prognostic parameters for OCA include:
- Patient age, tumor size, vascular invasion, extrathyroidal extension, and the presence of distant metastases:
- Distant metastases at diagnosis are the most important prognostic factor for OCA
- For OCA, the 5-year overall survival has been reported to be 85%:
- But only 24% among patients with distant metastases at diagnosis compared to 91% for patients with M0 disease at diagnosis
- Although it is not clear that OCA is more aggressive than follicular thyroid carcinoma after adjusting for variables such as patient age, gender, and tumor stage:
- Due to decreased efficacy of radioactive iodine with OCA compared to follicular thyroid carcinoma:
- Treating OCA is currently more difficult once there is disease recurrence
- Due to decreased efficacy of radioactive iodine with OCA compared to follicular thyroid carcinoma:
- Benign and malignant oncocytic thyroid tumors:
- Have both been shown to harbor homoplasmic or highly heteroplasmic (> 70%) mitochondrial DNA mutations in complex I subunit genes of the electron transport chain
- Additionally, OCAs demonstrate widespread chromosome losses that result in near-genome-wide haploidization with or without subsequent genome endoreduplication:
- Chromosomal changes have been found to be associated with extent of invasion:
- Most OCAs with capsular invasion only or focal vascular invasion have been shown to be diploid
- Whereas tumors with extensive vascular invasion and widely invasive tumors:
- Are usually polysomic and nearly always demonstrate chromosome 7 amplification
- Additionally, the near-haploid state has been shown to be maintained in metastases, implying selection during tumor evolution
- OCAs have also been shown to have recurrent DNA mutations, including RAS mutations (though at a lower rate than is seen with follicular thyroid carcinoma), EIF1AX, TERT, TP53, NF1, and CDKN1A, among others
- Chromosomal changes have been found to be associated with extent of invasion:
- Is used in the new World Health Organization (WHO) to refer to:

#Arrangoiz #Doctor #Surgeon #CancerSurgeon #HeadandNeckSurgeon #ThyroidSurgeon #SurgicalOncologist #ThyroidAwarenessMonth #ThyroidCancer #MountSinaiMedicalCenter #MSMC #Miami
