- Myth:
- Nipple wounds in lactating women should be treated with drying agents and topical antibiotics to prevent progression to mastitis
- Science:
- Surgical training provides strong education in wound care techniques and teaches the difference between traumatized versus infected tissue
- Surgeons debride devitalized tissue and understand the need to provide absorption for serous fluid and fibrinous exudate
- However, traditional lactation recommendations have contradicted principles of closed, moist healing for wound care
- Patients are often counseled to express a small amount of breastmilk onto nipple wounds and allow it to air dry
- They also may be recommended to soak nipples in Epsom salt or salt water and to use a hair dryer to prevent moisture build-up
- They are also often instructed to avoid wearing a bra or allow anything touch the nipples
- In addition, breastfeeding patients with nipple wounds are often warned they are at risk for ascending intraductal infection, that is, bacterial mastitis
- They are therefore encouraged to apply topical antibiotics to their wounds
- However, it is very uncommon for open, vascularized wounds to become secondarily infected in immunocompetent hosts
- Overutilization of antibiotics contributes to disruption of the microbiome and development of multidrug-resistant pathogens
- Routine use of topical antibiotics for open wounds is not recommended
- Furthermore, the hypothesis that bacterial mastitis is a result of ascending infection from nipple wounds is not supported by breast anatomy and physiology
- The highly vascular nature of the lactating breast and the multiple immune components of breastmilk prevent such infection
- Treatment:
- Care of the nipples include:
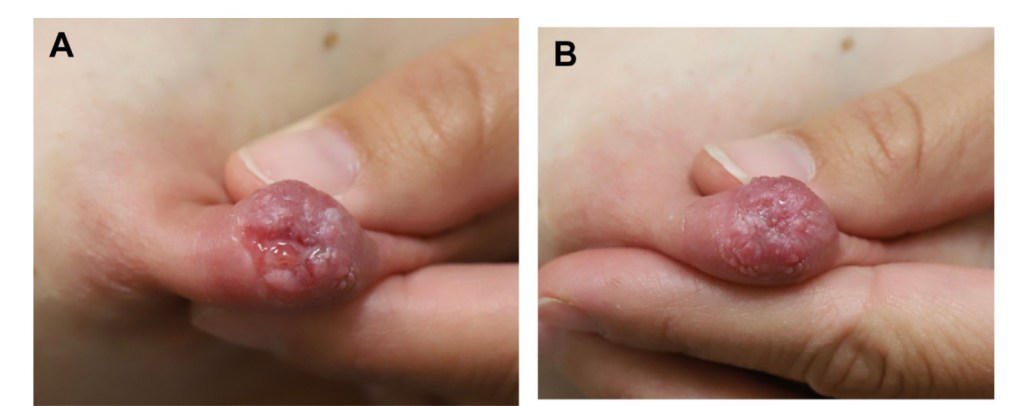
- Moist, closed wound healing principles should be followed, with the use of nonallergenic ointments / balms and sterile, absorbent dressings (Figure)
- Avoid ointments / balms containing potentially allergenic ingredients such as lanolin and petroleum
- APNO (All Purpose Nipple Ointment) should be avoided:
- This compounded prescription ointment contains an antifungal, antibacterial, and a steroid
- Although often recommended by lactation consultants and readily prescribed by the physicians to whom patients are referred, this nonspecific medication can cause additional complications
- Although patients may achieve some pain relief due to steroids and antiinflammatory properties of the antifungal, this potential benefit is outweighed by the risks of impaired wound healing from steroids and of microbiome disruption from nonselective elimination of normal flora
- Furthermore, other ingredients in this ointment may cause dermatitis
- This medication is generally expensive, even for patients with insurance
- Breast shells designed to “keep the nipple dry” or “protect the nipple from the bra” worsen swelling in the nipple, cause areola compression, and subsequently worsen pain
- Do not use drying agents such as antiseptics, alcohol, or Epsom salt soaks
- Similarly, do not use a hair dryer to blow hot, dehumidified air on nipples:
- These practices cause tissue desiccation, which is counterproductive for wound healing and increase the risk of skin breakdown
- Care of the nipples include:

#Arrangoiz #BreastSurgeon #CancerSurgeon #SurgicalOncologist #Surgeon #Surgeon #Doctor #MountSinaiMedicalCenter #MSMC #Miami #Mexico
