- In waveform analysis:
- The scalars of interest are:
- Volume vs time
- Pressure vs time
- Flow vs time
- The scalars of interest are:
- In volume assist control:
- It is common to have a constant flow pattern:
- Which will show up as straight in the flow scalar
- Adding an inspiratory pause (when flow = 0):
- Will indicate a plateau pressure in the pressure scalar
- In volume assist control:
- Effort will cause changes to the pressure waveform
- It is common to have a constant flow pattern:
- In pressure assist control:
- Pressure is held constant over time
- The rise time:
- Is the time it takes to reach the pressure provided during inspiration
- To find the plateau pressure:
- Use an inspiratory pause
- In pressure assist control:
- Effort by the patient will change the flow waveform
- To understand patient behavior:
- It is important to understand asynchrony, which includes:
- Neurological timing and ventilator timing:
- Is out of sync
- Neurological timing and ventilator timing:
- Flow starvation:
- The ventilator does not meet the demand of the patient
- Patient is unable to meet the trigger criteria
- It is important to understand asynchrony, which includes:
- In volume assist control:
- You will see patient effort:
- In the form of:
- Negative scooping:
- In the pressure waveform:
- If flow demand is not entirely met for the patient
- In the pressure waveform:
- Negative scooping:
- Patients with COVID-19:
- Often have excessive efforts when they interact with the ventilator
- As a result, it is important to monitor the occlusion pressure, or p0.1:
- To ensure it is not too high and to watch for significant scooping in the pressure waveform
- As a result, it is important to monitor the occlusion pressure, or p0.1:
- Often have excessive efforts when they interact with the ventilator
- In the form of:
- You will see patient effort:
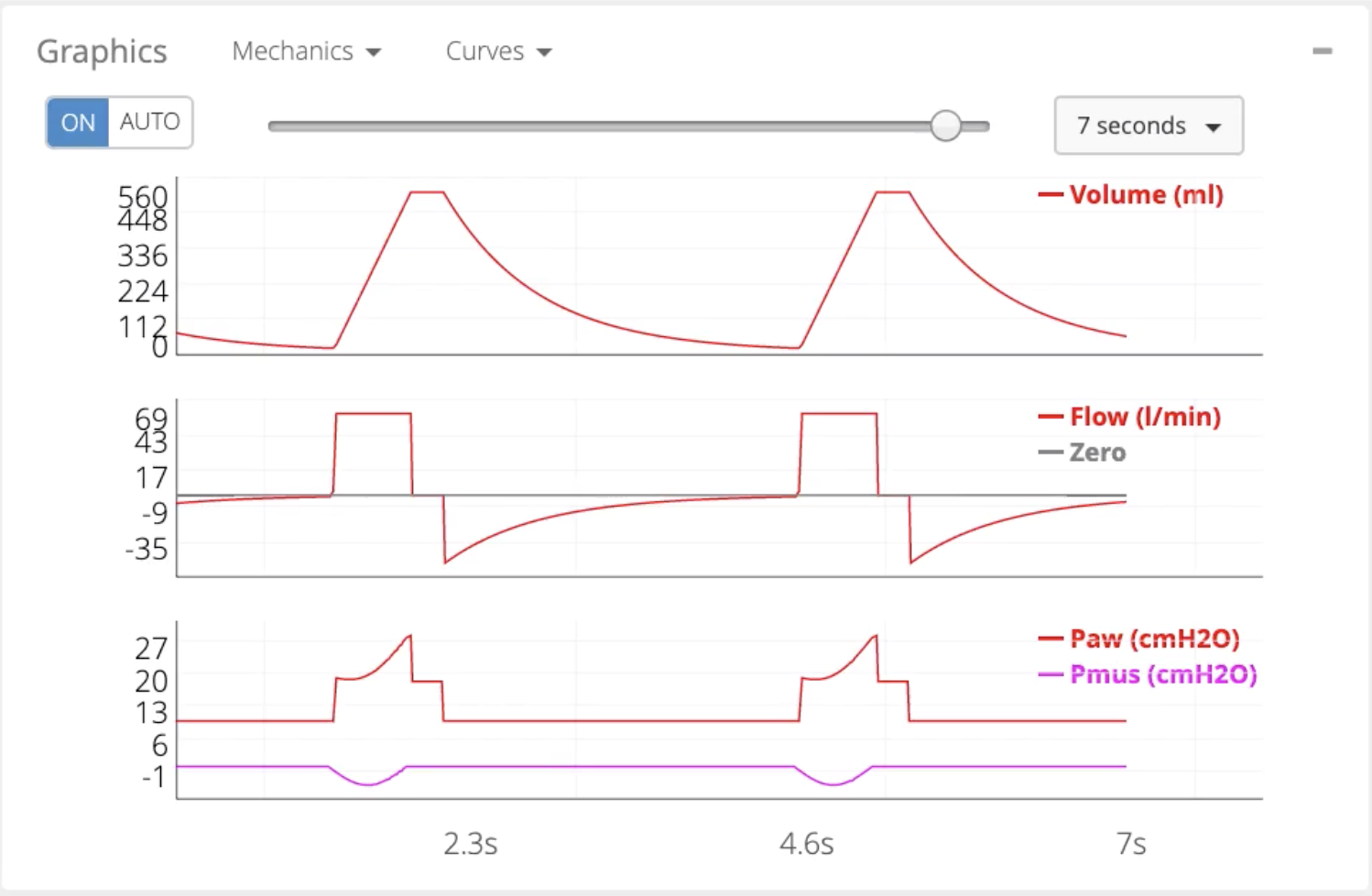
- The figure above shows patient effort in volume assist control with:
- A normal amount of scooping:
- With a p0.1 of 2.35 cmH2O
- A normal amount of scooping:
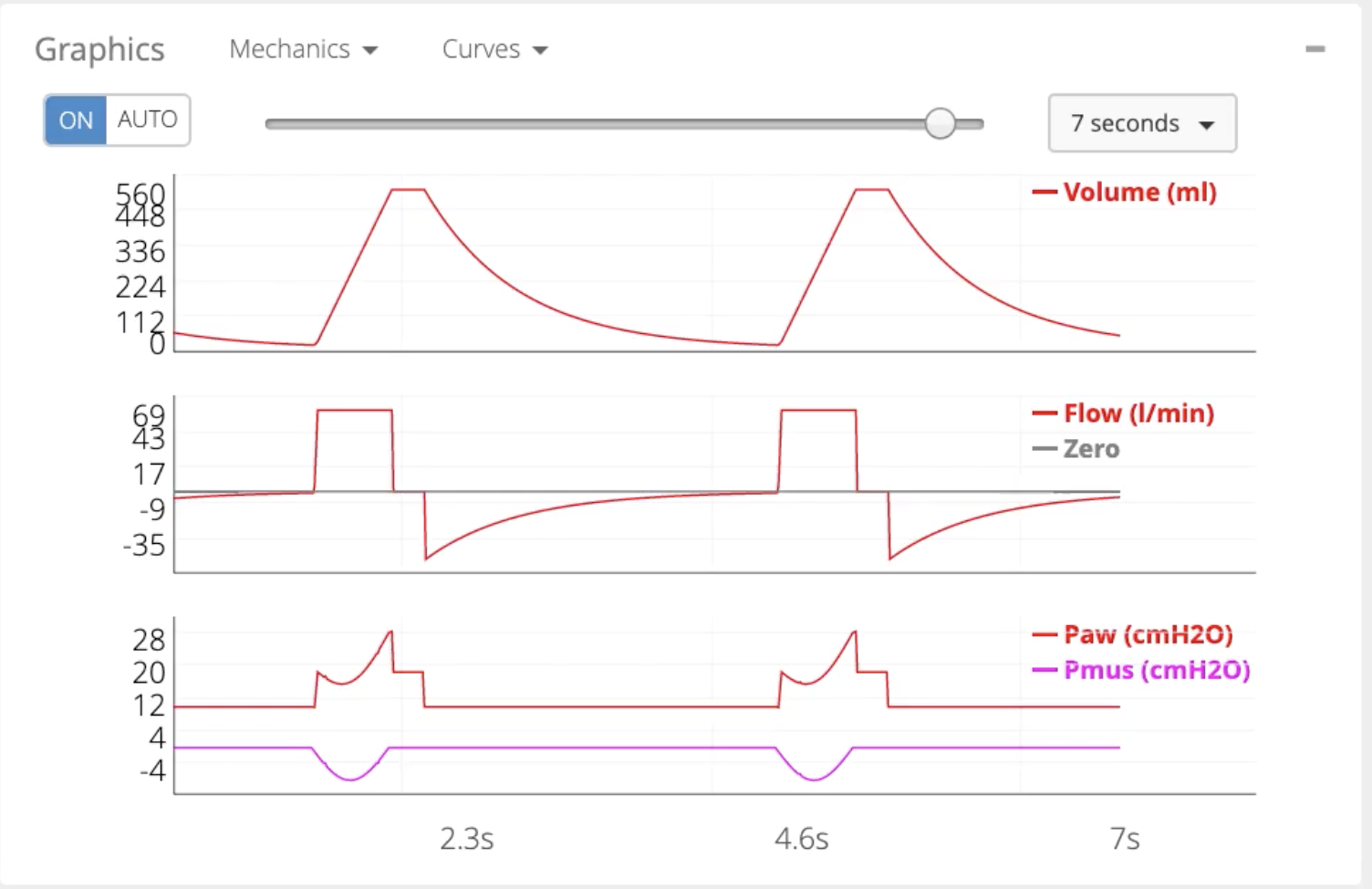
- The figure below indicates excessive effort:
- Which many COVID-19 patients display when they begin to interact with the ventilator:
- With p0.1 of 4.7
- Which many COVID-19 patients display when they begin to interact with the ventilator:
- In pressure assist control:
- Patient effort should change the:
- Flow waveform
- In this, it is important to check if the flow reaches 0 as pressure reaches 0:
- During inspiration or
- If there is dampening of the peak expiratory flow during exhalation:
- To ensure the patient is not experiencing asynchrony with breath timing:
- This can be adjusted by shortening or lengthening the inspiratory time
- Similarly, p0.1 can be monitored to evaluate whether a patient is experiencing excessive effort:
- In which increasing support should be done:
- In an attempt to reduce respiratory drive:
- Provided tidal volume is not excessive
- In an attempt to reduce respiratory drive:
- In which increasing support should be done:
- PEEP can also be adjusted to attempt to improve the patient’s drive
- To ensure the patient is not experiencing asynchrony with breath timing:
- In pressure support, it may be necessary to alter the % of peak inspiratory flow:
- That causes cycling off to eliminate asynchrony
- If the patient is demonstrating excessive effort:
- Increasing the pressure support:
- Will help decrease the patient’s drive:
- However, if increasing pressure support does not decrease the p0.1:
- Reducing the drive must be prioritized
- However, if increasing pressure support does not decrease the p0.1:
- Will help decrease the patient’s drive:
- PEEP can also be adjusted to attempt to improve the patient’s drive
- Increasing the pressure support:
- Patient effort should change the:
- Delayed cycling is another phenomena:
- Where the patient wants to exhale:
- But the machine has not cycled off yet
- In pressure assist control:
- If there is an increase in pressure at the end of inspiration with a subsequent rapid deceleration in the expiratory flow:
- Then the patient is most likely experiencing delayed cycling
- As a result, the inspiratory time should be shortened:
- However, the time should be not shortened so much that it causes premature cycling:
- In which the patient’s effort lasts longer than the ventilator’s cycle off criteria
- This will manifest as a dampening in the peak expiratory flow
- Premature cycling can also occur in pressure support:
- When the cycling-off percentage is too high:
- This flow scalar will look similar to that for premature cycling in pressure assist control
- When the cycling-off percentage is too high:
- However, the time should be not shortened so much that it causes premature cycling:
- If there is an increase in pressure at the end of inspiration with a subsequent rapid deceleration in the expiratory flow:
- Where the patient wants to exhale:
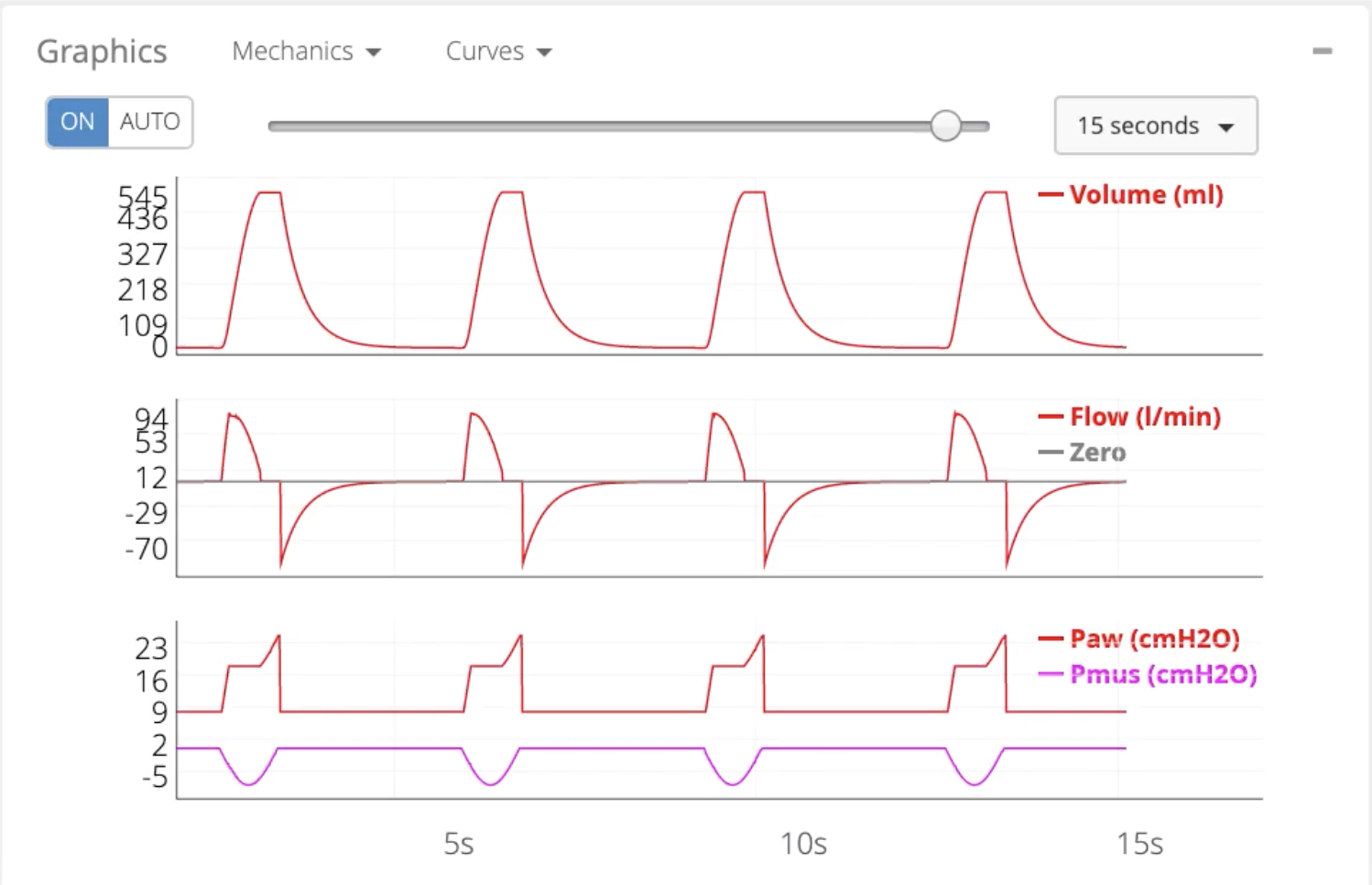
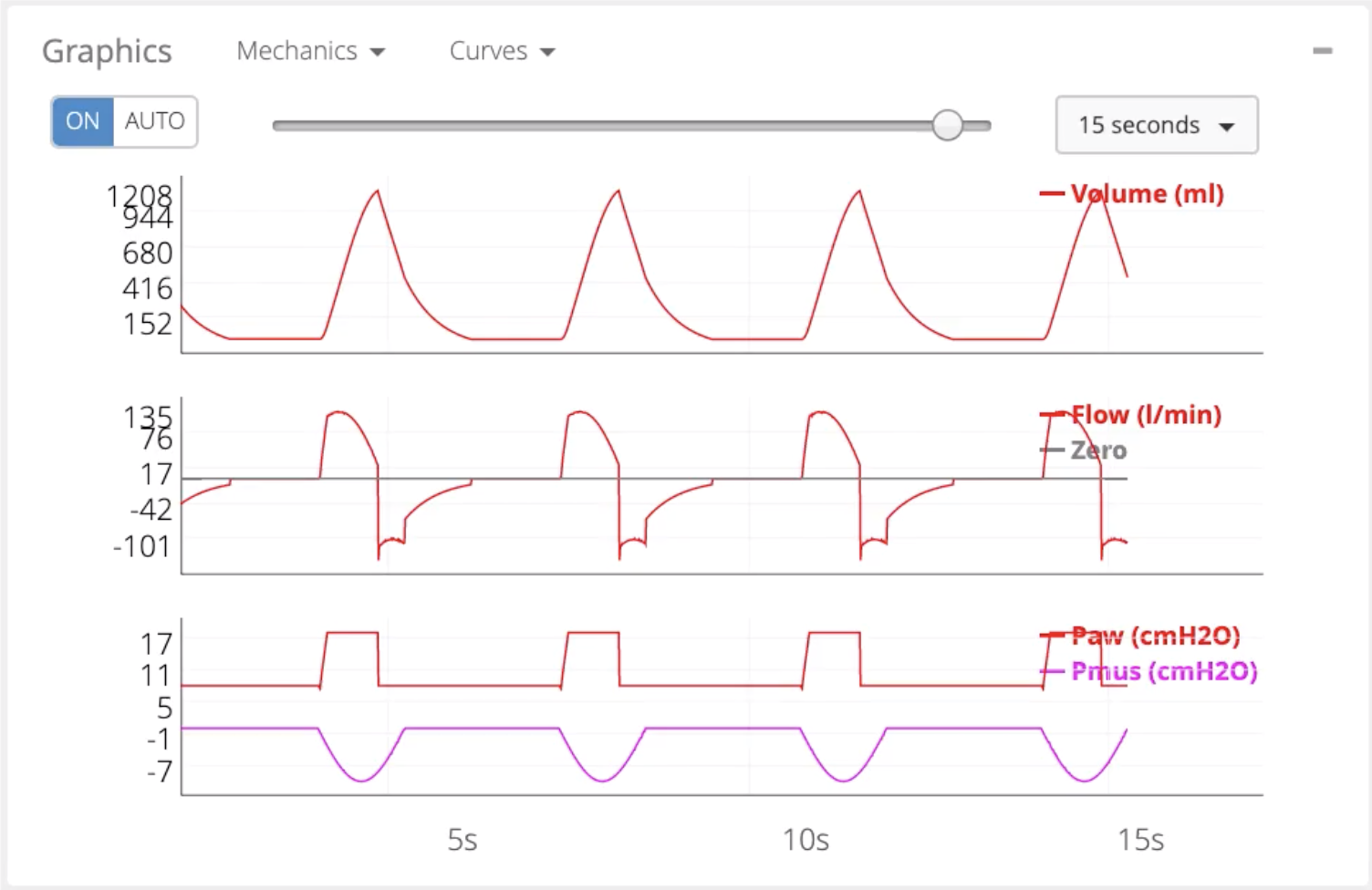
- In the figures above, delayed cycling (top) and premature cycling (bottom) in pressure assist control:
- Are noticeable by analyzing the flow scalar:
- The inspiratory time:
- Should be shortened for delayed cycling
- Lengthened in premature cycling
- The inspiratory time:
- Are noticeable by analyzing the flow scalar:
- Ineffective efforts are another form of asynchrony that generally occurs:
- When patients are overassisted (too much pressure support) or have too high of airway resistance:
- Delayed cycling is a common cause of ineffective efforts
- When patients are overassisted (too much pressure support) or have too high of airway resistance:
- Reverse triggering:
- Is another form of asynchrony:
- where the ventilator triggers a breath:
- That then triggers an effort from the patient:
- This can also lead to breath stacking
- That then triggers an effort from the patient:
- where the ventilator triggers a breath:
- The first thing to check when noting reverse triggering:
- Is to see if it is bad timing or reflex
- To check this:
- First reduce the respiratory rate
- After reducing the respiratory rate:
- If the patient is triggering the breaths, it was simply bad timing
- After reducing the respiratory rate:
- However, if the reverse triggering still continues, a few steps should be taken:
- Turn off sedation if possible
- Increase tidal volume to a maximum of 8 mL / kg of IBW
- Keep plateau pressure:
- Less than or equal to 27 cmH2O
- Less than 30cmH2O for COVID-19 patients:
- Typical ARDS guidelines
- If there is a known injurious pattern (breath stacking) and sedation cannot be stopped:
- Consider NMB agents to protect the lung and minimize the possibility of barotrauma
- First reduce the respiratory rate
- To check this:
- Is to see if it is bad timing or reflex
- Is another form of asynchrony:
#Arrangoiz #Surgeon #Teacher
