- The differential diagnosis of a small bowel mass:
- Is extensive
- Focal small bowel wall thickening can be present in:
- Bowel ischemia
- Inflammation:
- Inflammatory bowel disease
- Infection
- Radiation enteritis
- In addition to small bowel neoplasms
- Many of these conditions can be confirmed or excluded by:
- The history and physical examination
- Imaging characteristics
- Further studies:
- Endoscopy
- True small bowel masses can:
- Be either malignant or benign:
- Malignant lesions include:
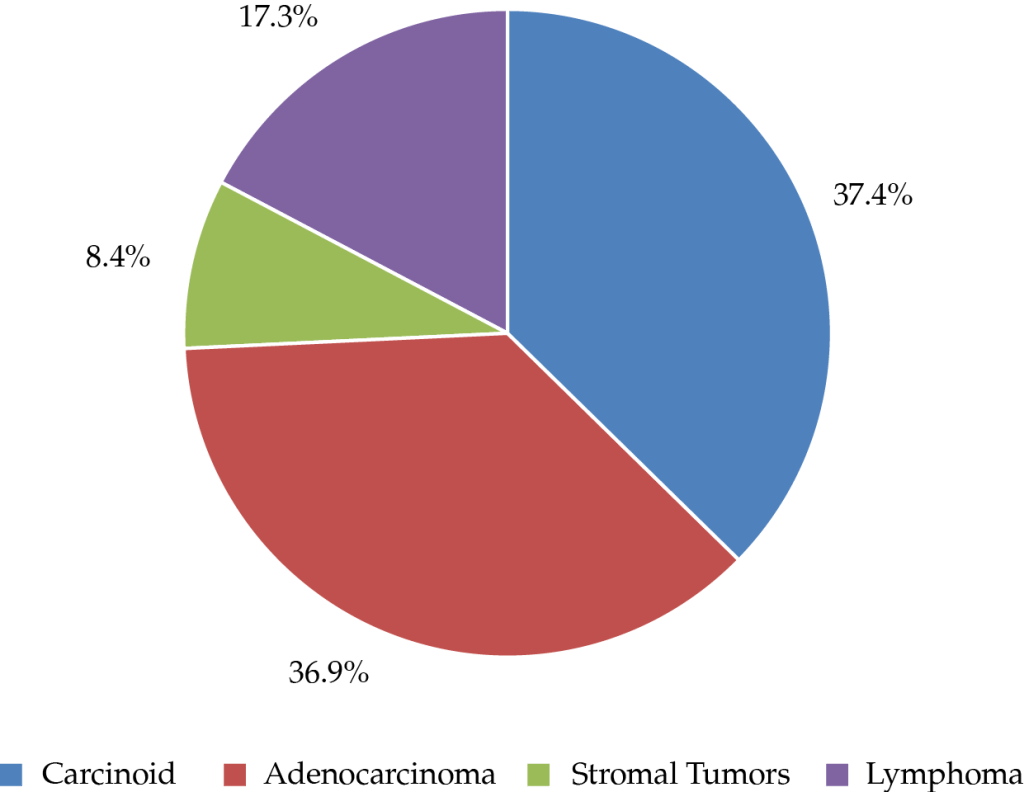
- Adenocarcinoma (36.9% of the cases)
- Carcinoid tumor (37.4% of the cases)
- Gastrointestinal stromal tumor (8.4% of the cases)
- Lymphoma (17.3% of the cases)
- Metastatic disease
- Malignant lesions include:
- Be either malignant or benign:
- The most common benign small bowel masses include:
- Adenomas
- Leiomyomas
- Lipomas
- More rare benign small bowel masses include:
- Fibromas
- Desmoids
- Hemangiomas
- Hamartomas
- Schwannomas
- Patients who present with:
- Obstruction, bleeding, or perforation from a small bowel mass:
- Typically require exploration and resection:
- Regardless of the etiology of the mass:
- Unless they are medically unfit for surgery
- Regardless of the etiology of the mass:
- Typically require exploration and resection:
- Obstruction, bleeding, or perforation from a small bowel mass:
- Patients who are asymptomatic or present with mild symptoms from a small bowel mass:
- Should be worked up further with:
- Tumor markers
- Endoscopic evaluation:
- For biopsy and tattoo if the lesion is endoscopically accessible:
- If the lesion is not endoscopically accessible:
- Then surgical resection:
- May be necessary for definitive diagnosis and treatment
- Then surgical resection:
- If the lesion is not endoscopically accessible:
- For biopsy and tattoo if the lesion is endoscopically accessible:
- Should be worked up further with:
Laboratory Test (Tumor Markers)
- Carcinoembryonic antigen (CEA):
- Is not sensitive or specific:
- For small bowel adenocarcinoma:
- But is elevated in 30% to 44% of those with:
- Advanced local or metastatic disease
- But is elevated in 30% to 44% of those with:
- For small bowel adenocarcinoma:
- Is not sensitive or specific:
- CA 19-9:
- Is also elevated in 30 % to 40% of those with:
- Advanced local or metastatic disease
- Is also elevated in 30 % to 40% of those with:
- These markers (CEA and CA 19-9) are best used:
- To raise suspicion:
- In patients being worked up for small bowel adenocarcinoma
- For surveillance:
- In those in whom it is elevated before treatment
- Given the high false negative rate:
- They should not be used to rule out adenocarcinoma
- To raise suspicion:
Imaging Work-Up
- Imaging is critical to differentiate a malignant etiology of nonspecific gastrointestinal symptoms from other causes:
- Nausea
- Vomiting
- Obstipation
- Bleeding
- Upper Gastrointestinal Series / Small Bowel Follow-through:
- An upper gastrointestinal series with small bowel follow-through has a relatively low sensitivity in the detection of small bowel tumors (< 60%):
- It is most commonly obtained in patients with a small bowel obstruction:
- To help ascertain the presence and location of a complete small bowel obstruction and may reveal:
- Intussusception
- Mucosal defect
- Tumor / mass:
- Which should prompt further (cross-sectional) imaging
- To help ascertain the presence and location of a complete small bowel obstruction and may reveal:
- It is most commonly obtained in patients with a small bowel obstruction:
- An upper gastrointestinal series with small bowel follow-through has a relatively low sensitivity in the detection of small bowel tumors (< 60%):
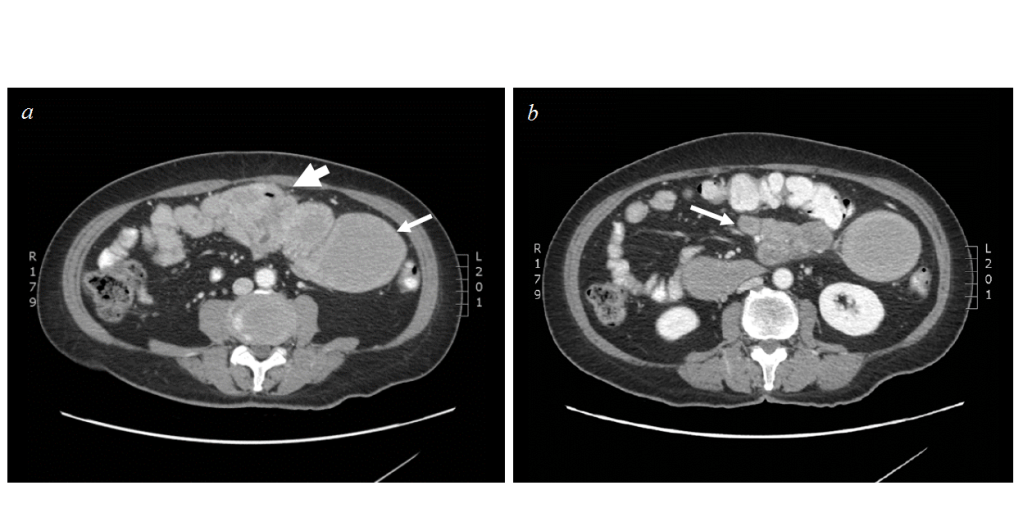
- Computed Tomography Scan:
- CT is useful to identify:
- Small bowel masses
- Nodal disease
- Distant metastases
- Alternative etiologies of abdominal symptoms
- Its sensitivity in detection of primary small bowel adenocarcinomas is:
- Approximately 80%
- CT appearance of small bowel adenocarcinoma includes:
- Demonstration of a discrete mass
- Focal mural thickening
- Small bowel obstruction
- Intussusception without a clear associated mass
- CT is useful to identify:
- PET can be useful to:
- Identify occult metastatic disease
- Increase the suspicion of malignancy:
- In nonspecific small bowel abnormalities on CT
- Enterography:
- Advanced cross-sectional imaging techniques, including:
- CT and magnetic resonance enterography:
- Can be more accurate than other imaging to confirm or exclude small bowel cancers:
- However, they are not universally available and have not been well studied in this population
- Can be more accurate than other imaging to confirm or exclude small bowel cancers:
- CT and magnetic resonance enterography:
- Advanced cross-sectional imaging techniques, including:
- Endoscopy:
- Endoscopic diagnosis of small bowel adenocarcinoma:
- Is often definitive:
- But is limited by the location of the tumor:
- Which must reside in an endoscopically accessible location
- But is limited by the location of the tumor:
- Because adenocarcinomas are mucosal tumors:
- They can often be visualized endoscopically:
- Assuming they can be reached
- They can often be visualized endoscopically:
- Endoscopy also allows biopsy to be performed and can tattoo a lesion that may not be visible externally during bowel resection
- Standard upper endoscopy is most useful if the suspected small bowel tumor is in the:
- Duodenum or proximal jejunum.
- Is often definitive:
- Endoscopic diagnosis of small bowel adenocarcinoma:
- Enteroscopy:
- Enteroscopy refers to upper endoscopy beyond the range of standard endoscopy:
- Into the proximal jejunum
- Techniques employed to advance the endoscope include:
- Push
- Balloon
- Intraoperative assistance
- Advantages over standard endoscopy include:
- Increased range:
- 50 cm to 150 cm distal to the ligament of Treitz
- Occasionally:
- The entire small bowel can be visualized using:
- Anterograde and retrograde (transanal) approaches
- The entire small bowel can be visualized using:
- Occasionally:
- 50 cm to 150 cm distal to the ligament of Treitz
- Increased range:
- Disadvantages include:
- Technical difficulty with a requisite learning curve
- iIncreased rates of:
- Pancreatitis
- Perforation:
- Over standard endoscopy
- Enteroscopy refers to upper endoscopy beyond the range of standard endoscopy:
- Wireless video capsule endoscopy:
- Wireless video capsule endoscopy is typically used to:
- Identify the source of occult gastrointestinal bleeding:
- But is infrequently used to visualize small bowel masses
- It has a high false negative rate (19%):
- In identifying small bowel masses:
- As well as a 2% false positive rate
- In identifying small bowel masses:
- Identify the source of occult gastrointestinal bleeding:
- Wireless capsule endoscopy:
- Also has no biopsy capability
- Can become lodged in nearly obstructing or obstructed segments of bowel
- Wireless video capsule endoscopy is typically used to:
#Arrangoiz #Surgeon #CancerSurgeon #SurgicalOncologist #Teacher #SmallBowelCancer
