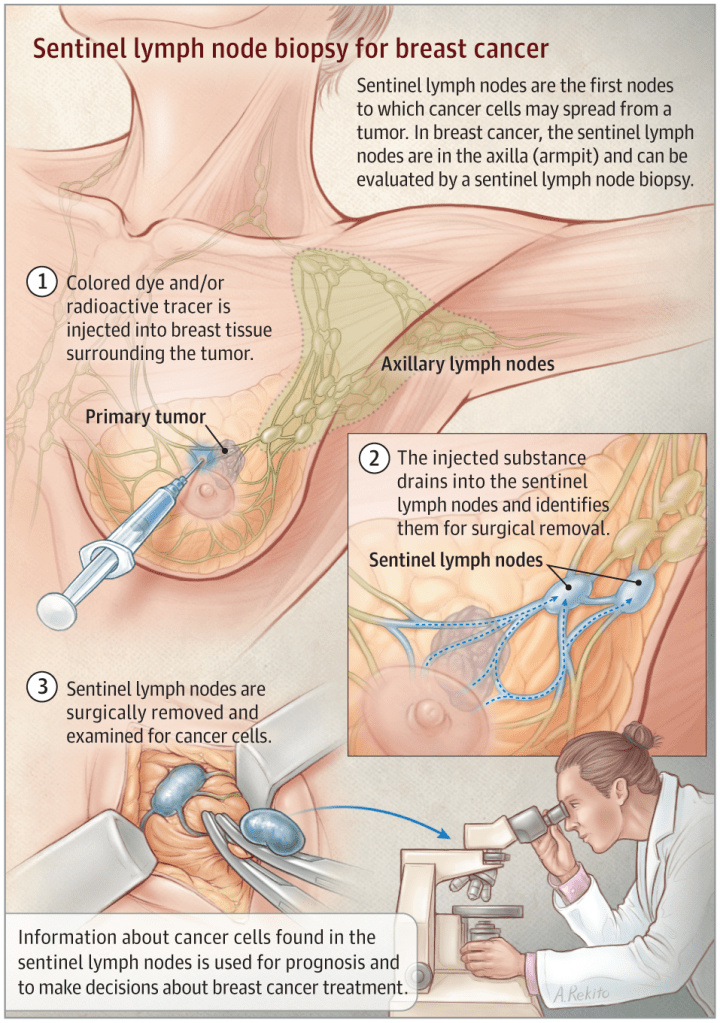
👉Krag et al. first described using technetium-99m sulfur colloid in sentinel node (SN) mapping and noted that he attained an SN identification rate of 98%, with a false-negative rate of 11%.
👉Technetium-99m sulfur colloid is the most widely used radioisotope for lymphatic mapping in the United States.
👉In Europe, technetium-99m colloid albumin is used most often.
👉Similarly, Giuliano et al. described the use of isosulfan blue dye, with a SN detection rate of 98%, without false-negative nodes.
👉Anaphylaxis and hypotension also have been reported as adverse events when using isosulfan blue dye.
👉Overall, isosulfan blue dye is the most commonly used dye for the lymphatic mapping of breast cancer.
👉The SN detection rate using methylene blue has been described as 93%, and concordance with radioisotope was described in 95% of patients.
👉Although methylene blue is available at a lower cost when compared to isosulfan blue, it must be injected carefully into the subcutaneous tissues.
👉Injection into the dermis may lead to epidermolysis and necrosis.
👉Therefore when used, methylene blue should be diluted with saline to minimize these complications (eg, 1 ml of 1% methylene blue diluted with 2 to 3 ml of injectable saline) and injected in the subareolar breast parenchyma deep to the skin.
👉The combination of blue dye and radioisotope improves the SN detection rate as first described by Albertini and colleagues.
👉As a result, several other studies have demonstrated similar findings and, thus, dual-agent lymphatic mapping has been accepted universally as a better method in the detection of the SN.
👉The National Surgical Adjuvant Breast and Bowel Project (NSABP) B-32 used radioisotope and blue dye for the detection of SLNs.
👉Sentinel nodes were identified by blue dye alone in 5.1%, by radioisotope alone in 24.3% and by both tracers in 65.1% of patients.
👉The reported SLN identification rate was 97% with a 9.8% false-negative rate.
The most common adverse events were allergic reactions.
👉Anaphylaxis was also reported as an adverse event.
REFERENCES
- Albertini JJ, Lyman GH, Cox C, et al. Lymphatic mapping and sentinel node biopsy in the patient with breast cancer. JAMA. 1996;276:1818-1822.
- Giuliano AE, Kirgan DM, Guenther JM, Morton DL. Lymphatic mapping and sentinel lymphadenectomy for breast cancer. Ann Surg. 1994;220:391-401.
- Kim T, Giuliano AE, Lyman GH. Lymphatic mapping and sentinel lymph node sampling in breast cancer: a meta-analysis. Cancer. 2006;106:4-16.
- Krag DN, Anderson SJ, Julian TB, et al. Sentinel-lymph-node resection compared with conventional axillary-lymph-node dissection in clinically node-negative patients with breast cancer: overall survival findings from the NSABP B-32 randomised phase 3 trial. Lancet Oncol. 2010;11:927-933.
- Krag DN, Weaver DL, Alex JC, Fairbank JT. Surgical resection and radiolocalization of the sentinel lymph node in breast cancer using a gamma probe. Surg Oncol. 1993;2:335-339.
- Newman LA, Newman EA. Lymphatic mapping techniques and sentinel lymph node biopsy. Surg Clin N Am. 2007;87:353-364.
- Simmons RM, Smith SM, Osborne MP. Methylene blue dye as an alternative to isosulfan blue dye for sentinel lymph node localization. Breast J. 2001;7:181-183.
- Simmons R, Thevarajah S, Brennan M, Christos P, Osborne M. Methylene blue dye as an alternative to isosulfan blue dye for sentinel node localization. Ann Surg Oncol. 2003;10:242-247.
- Zakaria S, Hoskin TL, Degnim AC. Safety and technical success of methylene blue dye for lymphatic mapping in breast cancer. Am J Surg. 2008;196:228-233.
#Arrangoiz #BreastSurgeon #BreastSurgeon
