
- The technique of subtotal thyroidectomy:
- Relied on the anatomical removal of visibly abnormal thyroid tissue.
- Leaving behind bilateral posterior remnants.
- The move to total thyroidectomy has meant not only that more thyroid tissue is removed, but that rather there has been a progressive awareness of the vagaries of embryological development of the thyroid, with dissection now focused on those changes in order to ensure completeness of resection, and thus efficacy of the procedure.
- Thyroid development involves the midline descent of thyroid tissue from the foramen caecum to the level of the larynx along the thyroglossal tract, at which stage the left and right lobes develop:
- What is not as well appreciated is that thyroid descent may well continue into the thyrothymic region (and even into the anterior mediastinum) forming a prolongation of thyroid tissue or even completely separate thyrothymic thyroid rests.
- In addition the lateral thyroid component arising from the 4th branchial cleft and ultimobranchial body fuses with the median component:
- To form the tubercle of Zuckerkandl:
- A distinct anatomical structure:
- This fusion is not only the source of the thyroid’s C-cells, but is also essential in the process of follicular development.
- A distinct anatomical structure:
- To form the tubercle of Zuckerkandl:
- Thyroglossal tract and pyramidal remnants:
- Routine dissection of the pyramidal area up to the laryngeal cartilage should be part of every total thyroidectomy:
- Even minimal recurrence in this area can be very apparent to the patient.
- More importantly, in patients with Graves’ disease:
- A small pyramidal lobe remnant can contain sufficient thyroid tissue to cause clinical recurrence even after an apparent ‘total’ thyroidectomy.
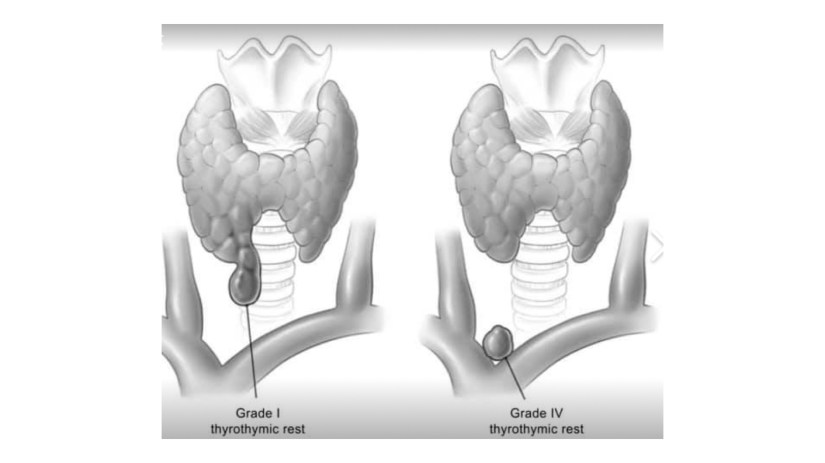
- Thyrothymic thyroid rests:
- Thyrothymic thyroid rests are present in over 50% of patients (if looked for), although most are small.
- They are often mistaken for small lymph nodes, or even parathyroid glands, and mostly cause no real problems.
- They are classified according to the nature of their connection to the thyroid gland proper:
- Grade I:
- Is a protrusion of thyroid tissue from the lower edge of the thyroid lobe.
- Grade II:
- Is a thyroid rest connected by a bridge of thyroid tissue
- Grade III:
- Is connected by only a fibrovascular core.
- Grade IV:
- Has no connection at all with the thyroid proper.
- Grade I:
- Their clinical significance lies in the fact that, if not removed at the initial operation, they may well reappear as retrosternal recurrence after apparent ‘total’ thyroidectomy:
- Routine dissection of the thyrothymic area down to the thoracic inlet looking for such rests should therefore be part of every total thyroidectomy.
- Routine dissection of the pyramidal area up to the laryngeal cartilage should be part of every total thyroidectomy:
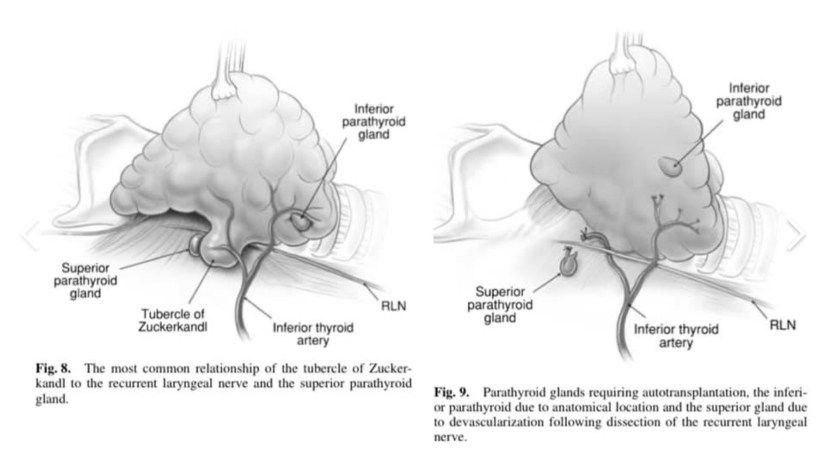
- The tubercle of Zuckerkandl:
- This structure, first described by Zuckerkandl in 1902, is a distinct anatomical entity, and can be found in nearly two-thirds of patients undergoing thyroid surgery.
- It is classified according to size (grades 0 to grade 3) using a system developed by Pelizzo et al.
- The tubercle of Zuckerkandl is often the source of local pressure or obstructive symptoms, especially when the thyroid itself is relatively small.
- The importance of the tubercle of Zuckerkandl, once again, is that if not looked for and removed during thyroid surgery:
- It may be a source of persistent unrelieved symptoms or recurrence.
- An understanding of the anatomy of the tubercle of Zuckerkandl is also central to safe surgical dissection:
- It usually enlarges lateral to the RLN, with the nerve appearing to pass into a cleft medial to it:
- A situation that some surgeons used to describe as the nerve passing into the thyroid substance.
- It usually enlarges lateral to the RLN, with the nerve appearing to pass into a cleft medial to it:
- Early elevation of the tubercle of Zuckerkandl usually allows the recurrent nerve to be easily and safely ‘encountered’ even though not initially visible.
- However:
- An uncommon but high risk situation is where the RLN runs lateral to an enlarged tubercle of Zuckerkandl, placing it at increased risk of damage during dissection.
- Another important point is that the normal superior parathyroid gland, also being derived from the fourth branchial cleft, is commonly found in close association, cephalad to the tubercle of Zuckerkandl.

- Introduction:
- Although the association between annual surgeon total thyroidectomy volume and clinical outcomes is well established, published methods typically group surgeons into volume categories.
- The volume-outcomes association is likely continuous, but little is known about the point at which the annual surgeon procedure volumes begin to be associated with a decrease in complication rates.
-
Multiple studies have demonstrated the relationship between surgeon volume and improved patient outcomes.
-
This is no different for thyroid surgery; when procedures are performed by high-volume surgeons, patients have decreased rates of endocrine-specific complications (e.g., transient and permanent hypoparathyroidism and recurrent laryngeal-nerve injury), shorter hospital stays, and lower rates of readmission.
-
Previous studies have varied with respect to the definition of a high-volume surgeon, ranging from a threshold of 30 to 100 thyroidectomies per year:
-
One recent study demonstrated that the likelihood of experiencing a complication decreased with increased surgeon volume, up to 26 total thyroidectomies per year.
-
-
The intent of the current study was to examine the association between surgeon volume and patient outcomes for total thyroidectomy, with the hypothesis that the optimal threshold is continuous, with no defined cut point defining a high-volume surgeon.
JAMA Otolaryngol Head Neck Surg. 2019 Jul 25. doi: 10.1001/jamaoto.2019.1752.
¿Quién debe realizar cirugía de tiroides?
- Generalmente debe ser cirujanos con sub-especialidades que tiene un volumen alto de casos por año:
- No es ideal un cirujano general que realizar muy pocos casos al año.
- Estas sub-especialidades son:
- Cirugia oncológica
- Cirugia de cabeza y cuello
- Cirugia endocrina
- Les dejo la respuesta de Ashok R. Shaha, MD, FACS (profesor MSKCC / IFHNOS) en su presentación que dio en el Keynote Lectura del American Head and Neck Society:

- Rodrigo Arrangoiz MS, MD, FACS miembro de Sociedad Quirúrgica S.C. cumple con los requisitos señalados por el Dr. Shaha:
- El Dr. Arrangoiz tiene entrenamiento en:
- Cirugía de tumores de cabeza y cuello, cirugía endocrina, y cirugía oncológica.
- Es pionero en México de la:
- Cirugia tiroidea minimamente invasiva
- La cirugia minimamente invasiva radio-guiada de paratiroides
- Cirugia tiroidea minimamente invasiva
- Es pionero en México de la:
- Cirugía de tumores de cabeza y cuello, cirugía endocrina, y cirugía oncológica.
- El Dr. Arrangoiz tiene entrenamiento en:
-
Su entrenamiento es el siguiente:
- Tumores de Cabeza y Cuello / Cirugía Endocrina:_
- Fox Chase Cancer Center
- Tumores de Cabeza y Cuello / Cirugía Endocrina:_

- Tumores de Cabeza y Cuello / Cirugía Endocrina:
- IFHNOS / Memorial Sloan Kettering Cancer Center
- Cirugía Oncológica Compleja:
- Fox Chase Cancer Center

- Cirugia General y Gastrointestinal:
- Michigan State University

- Maestría en Ciencias de Investigación:
- Drexel University

- El Dr. Arrangoiz esta certificado por:
- El Colegio Americano de Cirugía

- El Dr. Arrangoiz es:
- Fellow del Colegio Americano de Cirugía
- El Dr. Arrangoiz es:
- Fellow de la Sociedad de Cirugia Oncológica:
- Es miembro de la American Thyroid Association





