👉Cost savings from incorporating ThyroSeq testing into the management of patients with thyroid nodules with indeterminate cytology is based on the avoidance of unnecessary surgeries and selection of optimal extent for the initial surgery thereby minimizing the two-step surgeries, i.e. lobectomy followed by completion of thyroidectomy.
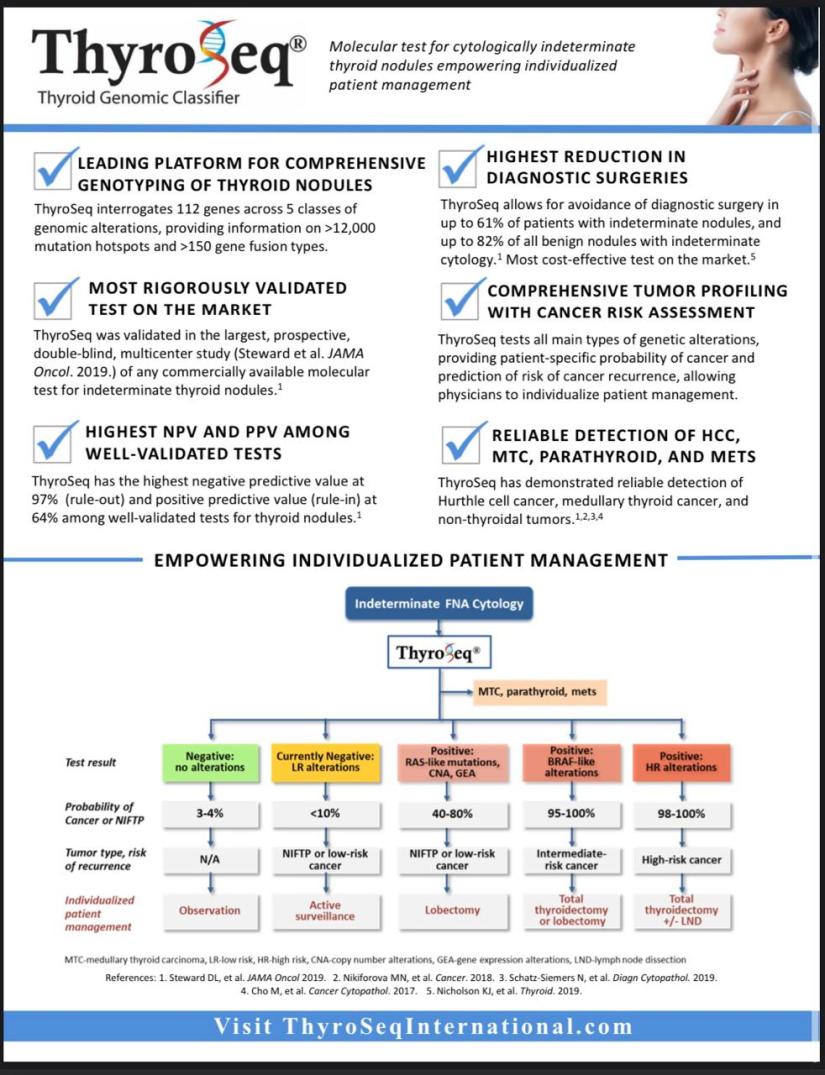
👉The results of a prospective, double-blind, multicenter study of ThyroSeq v3 (Steward DL et al. JAMA Oncol. 2018.) allow to estimate the impact of ThyroSeq on avoiding unneeded diagnostic thyroid surgeries, as show on the figure below.
👉In a series of 100 patients with Bethesda III and IV thyroid nodules and with the expected cancer/NIFTP prevalence of 28%, 61 tests will be reported as Negative and 39 as Positive. Among test-negative nodules only two cancers will be missed (those are expected to be low-risk, intrathyroidal cancers).
👉Among test-positive nodules, 23 (67%) will be diagnosed as cancer or NIFTP on surgery, and the majority of remaining nodules are expected to be neoplasms, likely with some malignant potential.
👉Overall, 61% of thyroid surgeries will be avoided, with their costs and complications.

👉This study modeled a decision tree from the payor perspective, comparing the cost-effectiveness of diagnostic lobectomy, ThyroSeq v3, and Afirma GSC for indeterminate (Bethesda III/IV) thyroid nodules.
👉Based on the model, the cost per correct diagnosis was $14,277 for ThyroSeq v3, $17,873 for Afirma GSC, and $38,408 for diagnostic lobectomy.
👉One-way sensitivity analysis found that ThyroSeq v3 had robustly lower cost per correct diagnosis than Afirma GSC.
👉Two-way sensitivity analysis varying costs of ThyroSeq v3 and Afirma GSC demonstrated that ThyroSeq was still the preferred strategy.
👉The study stated that in no range of tested cost variations was diagnostic lobectomy the preferred strategy over molecular testing.
👉The study concluded that either Afirma GSC or ThyroSeq v3 was considerably more cost-effective than diagnostic lobectomy and that ThyroSeq v3 was more likely to be cost-effective than Afirma GSC.

👉This study evaluated cost effectiveness of ThyroSeq utilized for managing patients with Bethesda III-IV cytology nodules at Mayo Clinic Florida, where the test is used in routine clinical practice since January 2015.
👉The study showed that the cost of treatment per patient with Bethesda III category nodules was $54,000 when no molecular testing was used and $44,570 after ThyroSeq introduction.
👉Three patients with negative ThyroSeq results were able to avoid surgery resulting in cost saving of $67,500 per patient.
👉For patients with Bethesda IV category nodules, the cost of treatment was $29,000 and $43,200 using and not using ThyroSeq, respectively.
👉Twelve patients with Bethesda IV nodules were negative by ThyroSeq, of which 11 did not have surgery, resulting in cost saving of $84,000 per patient.
👉The authors of this independent study performed at a high volume thyroid medical center concluded that ThyroSeq is a cost effective tool to diagnose thyroid cancer compared to thyroidectomy without molecular testing in patients with nodules categorized as Bethesda III and IV.
👉This study evaluated the costs associates with management of patients with Bethesda IV cytology nodule using ThyroSeq as compared to standard of care (SC) patient management without molecular testing, using Afirma®GEC, and using 7-gene mutational panel.
👉The study demonstrated that the ThyroSeq-guided care was associated with a substantially lower cost (average per patient $7,683, range $7,174-$8,333) as compared to the average per patient cost of standard of care ($11,505, range $10,676-$12,347) and of care utilizing Afirma®GEC ($13,027, range $12,373-$13,666) or 7-gene mutational panel ($12,029, range $11,254-$12,823). The study estimated that due to high test sensitivity (90%) and specificity (93%), ThyroSeq GC-guided algorithm for Bethesda IV nodules should result in 30% reduction in the average per patient cost of management of patients with these nodules.
- What is Head and Neck Surgery?:
- It is a surgical sub-specialty that deals mainly with benign and malignant tumors of the head and neck region, including:
- The scalp, facial region, eyes, ears, nose, nasal fossae, paranasal sinuses, oral cavity, pharynx (nasopharynx, oropharynx, hypopharynx), larynx (supraglotic larynx, glottis larynx, subglotic larynx), thyroid gland, parathyroid gland, salivary glands (parotid glands, submandibular glands, sublingual glands, minor salivary glands), soft tissues of the neck, skin of the head and neck region.
- The head and neck surgeon’s work area:
- Does not cover tumors or diseases of the brain and other areas of the central nervous system or those of the cervical spine:
- This is the neurosurgeon field.
- Does not cover tumors or diseases of the brain and other areas of the central nervous system or those of the cervical spine:
- The head and neck surgeon’s work area:
- The scalp, facial region, eyes, ears, nose, nasal fossae, paranasal sinuses, oral cavity, pharynx (nasopharynx, oropharynx, hypopharynx), larynx (supraglotic larynx, glottis larynx, subglotic larynx), thyroid gland, parathyroid gland, salivary glands (parotid glands, submandibular glands, sublingual glands, minor salivary glands), soft tissues of the neck, skin of the head and neck region.
- Among the diagnostic procedures performed by the head and neck surgeon, are the following:
- Nasopharyngolaryngoscopy:
- Performed to examine, evaluate and, possibly perform a biopsy, of oral cavity, pharyngeal and laryngeal lesions.
- Nasopharyngolaryngoscopy:
- The surgeries most commonly performed by the head and neck surgeon are:
- Total or near total thyroidectomies
- Hemithryoidectomies (lobectomies)
- Comprehensive neck dissections
- Selective neck dissections
- Maxillectomies:
- Total maxillectomy
- Subtotal maxillectomy
- Infrastructure maxillectomy
- Suprastructure maxillectomy
- Medial maxillectomy
- Mandibulectomy:
- Segmental
- Marginal
- Tracheostomy
- Salivary gland surgeries:
- Parotid gland operations:
- Limited superficial parotidectomy with identification and preservation of the facial nerve
- Superficial parotidectomy with identification and preservation of the facial nerve
- Near total parotidectomy with identification and preservation of the facial nerve
- Total parotidectomy
- Submandibular gland resection
- Sublingual gland resection
- Parotid gland operations:
- Resection of tumors of the oral cavity:
- Glossectomy
- Resection of the floor of the mouth tumors
- Resection of tumors of the pharynx
- Resection of tumors of the larynx
- Split-thickness skin grafts
- Full-thickness skin grafts
- Sentinel lymph node mapping and sentinel lymph node biopsy
- Resection of malignant skin tumors (BCC, SCC, melanoma) of the head and neck region
- It is a surgical sub-specialty that deals mainly with benign and malignant tumors of the head and neck region, including:
- The formation of the head and neck surgeon includes mastering the following subjects:
- Surgical Anatomy
- History and Basic Principles of Head and Neck Surgery
- Epidemiology, Etiology, and Pathology of Head and Neck Diseases
- Diagnostic Radiology of the Head and Neck Region
- Tumors of the Scalp, Skin and Melanoma
- Eyelids and Orbit
- Nasal Cavity and Paranasal Sinuses
- Skull Base and Temporal Bone
- Lips and Oral Cavity
- Pharynx and Esophagus
- Larynx and Trachea
- Cervical Lymph Nodes
- Thyroid and Parathyroid Glands
- Salivary Glands
- Neurogenic Tumors and Paragangliomas
- Soft Tissue Tumors
- Bone Tumors and Odontogenic Lesions
- Reconstructive Surgery
- Oncologic Dentistry and Maxillofacial Prosthetics
- Principles of Radiation Oncology
- Principles of Chemotherapy
- Molecular Oncology, Genomics and Immunology
- Nutrition
- Biostatistic
Rodrigo Arrangoiz MS, MD, FACS a head and neck surgeon / endocrine surgeon / surgical oncologist and is a member of Sociedad Quirúrgica S.C at the America British Cowdray Medical Center in Mexico City:





