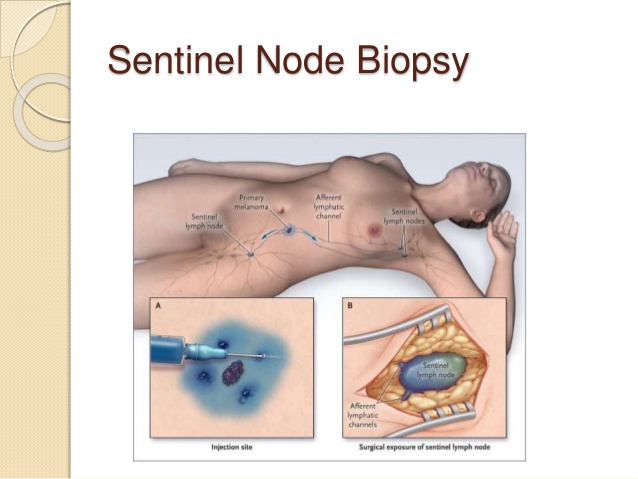


👉Although neoadjuvant chemotherapy (NAC) can decrease the size of a primary tumor to allow for breast conservation, eliminate nodal metastasis in some patients, and provide prognostic information, the optimal timing of SLNB for patients treated with NAC has been controversial.
👉Clinical staging of the axilla with SLNB is feasible both before and after chemotherapy.
👉SLNB prior to NAC may be a more accurate approach than after NAC.
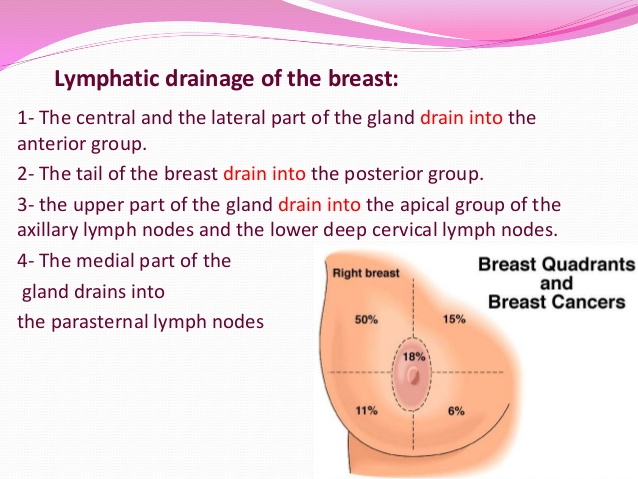
👉Chemotherapy may alter lymphatic drainage through fibrosis of lymphatic channels and decreases the accuracy of SLNB.
👉SLNB before NAC has a lower false negative rate and provides more accurate staging, which could determine radiation fields.
👉Unfortunately, SLNB prior to NAC requires an additional operation, could delay the initiation of chemotherapy, and fails to decrease the rate of ALND.
👉It also eliminates prognostic information given by the effect of chemotherapy on axillary metastasis. Ç
👉These concerns have led to interest in performing SLNB after NAC.
👉Several recent prospective trials have examined the accuracy of SLNB after NAC.
👉The American College of Surgeons Oncology Group (ACOSOG) Z1071 enrolled women with cT0 to cT4, cN1 to cN2 clinical disease who underwent neoadjuvant chemotherapy.
👉 All patients underwent pre-NAC axillary needle biopsy.
👉41% of patients had a pathologic complete response (PCR) in the axilla.
👉After chemotherapy, patients underwent both SLNB and ALND.
👉A sentinel lymph node could not be identified in 7% of patients.
👉The overall false negative rate was 13%, which did not meet the preset target of 10%.
👉The false negative rate was 21% in patients with two or fewer sentinel lymph nodes identified but dropped to 9.1% when greater than three sentinel lymph nodes were sampled.
👉In the Sentinel Lymph Node Biopsy in Patients with Breast Cancer Before and After Neoadjuvant Chemotherapy (SENTINA) trial, 1,022 patients underwent SLNB before NAC, with a detection rate of 99%.
👉As seen in ACOSOG Z1071, the false negative rate was much higher in patients with only one node removed (24%) than in those with three or more sentinel nodes removed (7%).
👉The false negative rate was also improved by the use of radiocolloid and blue dye together compared with blue dye alone (false negative rate of 9% versus 16%).
👉The Sentinel Node Biopsy following NeoAdjuvant Chemotherapy (SN FNAC) study enrolled patients with cT0 to cT3 with cN1 to cN2 biopsy-proven breast cancer treated with NAC.
👉The overall post-NAC SLNB false negative rate was 8% in 153 patients.
👉When only one sentinel lymph node was evaluated, the false negative rate was again unacceptably high at 20%.
👉On the basis of these three trials, resecting only one sentinel node is associated with an unacceptably high false negative rate (between 22% to 24%).
👉The false negative rate after NAC may be lowered with the use of dual tracers (from 16% to 9%) and resecting three or more sentinel nodes.
👉The sentinel lymph node identification rate after NAC is significantly improved with increased surgeon experience, suggesting that a learning curve is needed to obtain accurate SLNB after NAC.
👉SLNB after NAC has the potential to decrease the number of women who receive ALND.
👉A study of 288 prospectively identified clinically node-positive patients reported that 132 became clinically node negative after NAC.
👉The clinically node-negative patients were then eligible for SLNB, and 48% had negative sentinel lymph nodes and were able to avoid an ALND.
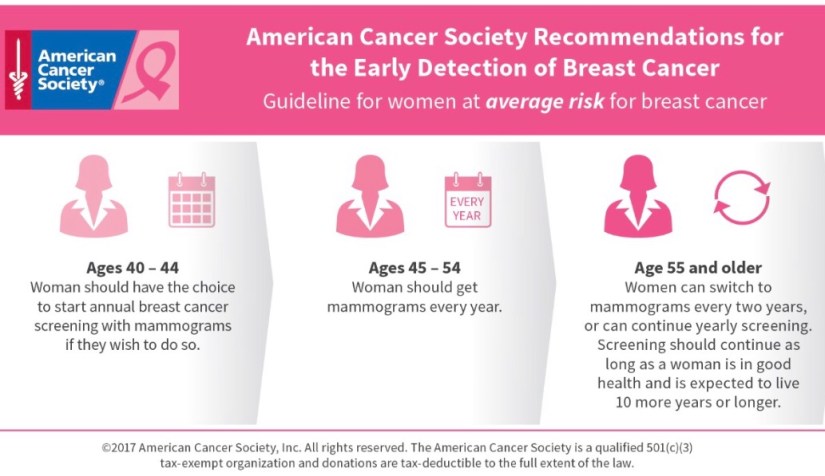
👉Current ASCO recommendations state that SLNB should be offered to patients who have received preoperative neoadjuvant systemic therapy and have clinically negative lymph nodes.
👉However, no large studies have examined local recurrence rates or survival when ALND is omitted in patients who convert from node positive to node negative after NAC.
👉The safety of avoiding ALND in these patients has not been demonstrated.
👉The National Surgical Adjuvant Breast and Bowel Project (NSABP) B51 and Alliance A011202 are two sister studies examining the role of SLNB, ALND, and nodal radiation in patients who receive NAC.
👉The results of these trials will help identify patients who can safely avoid ALND after NAC.
 Rodrigo Arrangoiz MS, MD, FACScirujano oncology y miembro de Sociedad Quirúrgica S.C en el America British Cowdray Medical Center en la ciudad de Mexico:
Rodrigo Arrangoiz MS, MD, FACScirujano oncology y miembro de Sociedad Quirúrgica S.C en el America British Cowdray Medical Center en la ciudad de Mexico:
-
Es experto en el manejo del cáncer de mama.

Training:
• General surgery:
• Michigan State University:
• 2004 al 2010
• Surgical Oncology / Head and Neck Surgery / Endocrine Surgery:
• Fox Chase Cancer Center (Filadelfia):
• 2010 al 2012
• Masters in Science (Clinical research for health professionals):
• Drexel University (Filadelfia):
• 2010 al 2012
• Surgical Oncology / Head and Neck Surgery / Endocrine Surgery:
• IFHNOS / Memorial Sloan Kettering Cancer Center:
• 2014 al 2016