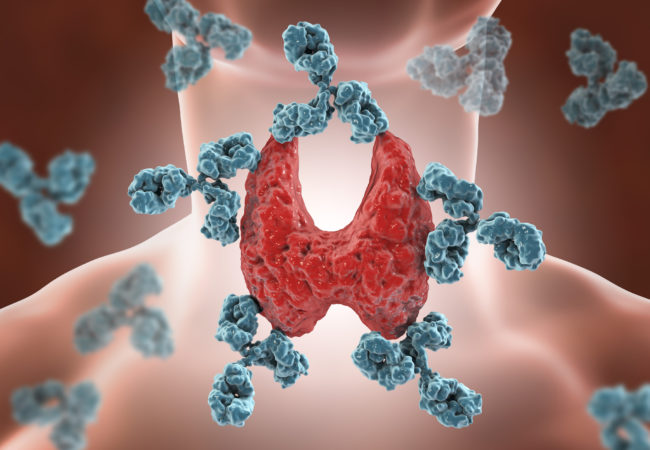
- Hashimoto’s thyroiditis (HT), a common autoimmune disease:
- Is the most frequent cause of hypothyroidism:
- Affecting 2% to 15% of the population.
- Histologically, HT is characterized by:
- Diffuse lymphocytic infiltration of the thyroid gland.
- It has been hypothesized that HT:
- A chronic thyroid inflammatory disease accompanied by positive serum thyroid peroxidase antibody (TPOAb) titers:
- Is associated with an increased risk of thyroid cancer:
- However, previous studies have not been able to prove this conclusively.
- Is associated with an increased risk of thyroid cancer:
- A chronic thyroid inflammatory disease accompanied by positive serum thyroid peroxidase antibody (TPOAb) titers:
- Is the most frequent cause of hypothyroidism:
- THYROID CANCER – Clinical THYROIDOLOGY ® ISSN: 2329-9711 | AUGUST 2019 | VOLUME 31 | ISSUE 8:
- Clin Thyroidol 2019;31:333–335:
- Hashimoto’s Thyroiditis Is a Risk Factor for Thyroid Cancer:
-
- Review of:
- Silva de Morais N, Stuart J, Guan H, Wang Z, Cibas ES, Frates MC, Benson CB, Cho NL, Nehs MA, Alexander CA, Marqusee E, Kim MI, Lorch JH, Barletta JA, Angell TE, Alexander EK 2019 The impact of Hashimoto thyroiditis on thyroid nodule cytology and risk of thyroid Cancer. J Endocr Soc 3:791–800. PMID: 30963137
- Review of:
-
- METHODS:
- Prospective cohort study of 10,054 consecutive adult patients with thyroid nodules greater 1 cm who were evaluated between 1995 and 2017 at the Brigham and Women’s Hospital Thyroid Nodule Clinic.
- All patients underwent sonographic and clinical assessment.
- From the ultrasound report, HT was considered present if the background parenchyma was diffusely heterogeneous or the presence of HT was reported.
- Serum TPOAb levels were measured (n = 2551 patients) when the serum TSH level was elevated or at the discretion of the clinician.
- The TPOAb test was considered positive when the antibody level was above the reference range.
- Thyroid nodules were treated according to the clinical guidelines at the time of evaluation.
- Fine-needle aspiration (FNA) was performed with ultrasound guidance when indicated.
- FNA specimens were processed using ThinPrep liquid-based cytology preparation.
- Thyroid cytology was reported as non-diagnostic, negative for malignant cells, atypia of undetermined significance, suspicious for follicular or Hürthle-cell neoplasm, suspicious for malignancy, or malignant.
- Surgery was recommended if cytologic findings were suspicious for malignancy or malignant.
- When thyroidectomy was performed (n = 3186 patients), histopathologic data were obtained to document malignant or benign disease as well as histologic evidence of HT.
- Hashimoto’s Thyroiditis Is a Risk Factor for Thyroid Cancer:
- Clin Thyroidol 2019;31:333–335:
- RESULTS:
- The final cohort included 9851 patients with 21,397 nodules.
- The population was predominantly female (83.9%) with a mean age of 52.2 years.
- A total of 14,063 (66%) of the nodules were evaluated with FNA.
- HT was diagnosed in 2651 patients (27%) with a total of 3895 nodules.
- The proportion of nodules with indeterminate and malignant cytology was higher in the HT group as compared with the non-HT group:
- Indeterminate cytology was found in:
- 20.6% of HT patients with nodules, while it was identified in only 17.1% of non-HT patients (P<0.01).
- Cancer was diagnosed on histopathology more frequently in the HT patients as compared with the non-HT patients: 23.3% vs. 15.9%, P<0.01.
- There were no significant differences in pathologic characteristics or markers of aggressiveness between the two groups.
- Indeterminate cytology was found in:
- Of note, 13 cases of thyroid lymphoma were identified (9 in patients without HT and 4 in patients with HT).
- CONCLUISON:
- In patients with thyroid nodules, HT is associated with a higher rate of indeterminate cytology and a higher incidence of thyroid malignancy:
- Assessment of HT is an important part of a thyroid nodule evaluation.
- In patients with thyroid nodules, HT is associated with a higher rate of indeterminate cytology and a higher incidence of thyroid malignancy:
- COMMENTARY:
- The results of previous studies have been inconclusive.
- In this study, the investigators evaluated a very large cohort of patients prospectively.
- The patient population was selected based on the presence of a clinically significant thyroid nodule:
- Thus, it does not represent the general population.
- But, based on these results, it appears that a nodule in a patient with HT is more likely to be thyroid cancer.
- This is a clinically significant finding as both HT and thyroid nodules are so common.
- It may be necessary to consider thyroid ultrasound in all HT patients to evaluate for the presence of thyroid nodules.
Sociedad Quirúrgica S.C tiene un experto en el manejo del cáncer de tiroides:
- Rodrigo Arrangoiz MS, MD, FACS

-
Entrenamiento:
• General surgery:
• Michigan State University:
• 2004 al 2010
• Surgical Oncology / Head and Neck Surgery / Endocrine Surgery:
• Fox Chase Cancer Center (Filadelfia):
• 2010 al 2012
• Masters in Science (Clinical research for health professionals):
• Drexel University (Filadelfia):
• 2010 al 2012
• Surgical Oncology / Head and Neck Surgery / Endocrine Surgery:
• IFHNOS / Memorial Sloan Kettering Cancer Center:
• 2014 al 2016
#Arrangoiz
#Teacher
#Surgeon
#Cirujano
#ThyroidExpert
#ThyroidSurgeon
#CirujanodeTiroides
#ExpertoenTiroides
#ExpertoenParatiroides
#Paratiroides
#Hiperparatiroidismo
#CancerdeTiroides
#ThyroidCancer
#PapillaryThyroidCancer
#SurgicalOncologist
#CirujanoOncologo
#CancerSurgeon
#CirujanodeCancer
#HeadandNeckSurgeon
#CirugiaEndocrina
#CirujanodeTumoresdeCabezayCuello
#OralCavityCancer
#Melanoma




