Introduction
- Primary hyperparathyroidism (PHPT) is caused by increased secretion of parathyroid hormone (PTH) by the parathyroid gland(s):
- Which leads to an elevated serum calcium level.
- Single gland disease:
- Caused by a single, enlarged, overactive gland:
- Is found in over 85% to 90% of the cases.
- Multiple gland disease occurs in 10% to 15% of cases:
- Multiple gland disease may consist of:
- Double adenomas:
- 6% to 9% of the cases
- Four-gland hyperplasia
- 3% of the cases
- Three enlarged and one normal appearing gland:
- 0.3% of the cases.
- Double adenomas:
- Because asymmetric hyperplasia is common:
- It is difficult to distinguish between multiple adenomas and hyperplasia and the term multiple gland disease is preferred.
- Multiple gland disease may consist of:
- Caused by a single, enlarged, overactive gland:
- PHPT in the United States usually presents quite early:
- Often when hypercalcemia is noted during routine laboratory testing and the patients has minimal symptoms.
- Signs may include:
- Nephrolithiasis (kidney stones)
- Decreased bone density (osteopenia or osteoporosis)
- Fragility fractures
- Subjective symptoms may include:
- Fatigue, cognitive changes, depression, emotional lability, anxiety, irritability, decrease social interaction, constipation and other gastrointestinal complaints (abdominal pain, nausea, anorexia, GERD), musculoskeletal pain, point pain, bone pain nocturia, muscle weakness and rarely pruritus.
- Most patients will be symptomatic if a detailed history is performed.
- A family history of endocrine disorders should be investigated, as hyperparathyroidism alone can be familial or can present as a component of multiple endocrine neoplasia (MEN) types 1 and 2A.
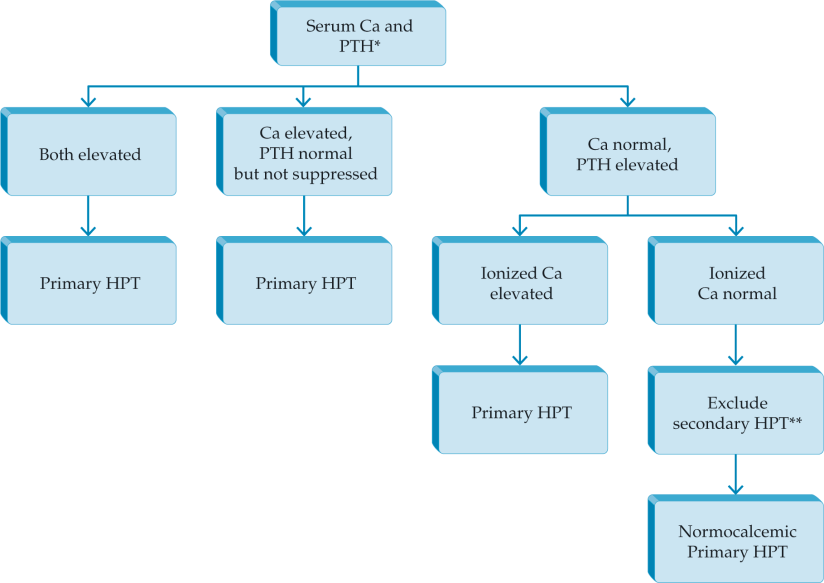
Diagnostic Evaluation
- A biochemistry panel consisting of:
- Serum total calcium, PTH level, creatinine, and 25-OH vitamin D should be obtained.
- An inappropriately elevated PTH level is the disease hallmark on laboratory examination.
- Calcium and PTH are tightly regulated and need to be evaluated concurrently when considering hyperparathyroidism

- In a patient with hypercalcemia:
- A PTH level at the upper normal range is inappropriately elevated and indicative of PHPT.
- Normocalcemic PHPT is a condition characterized by a:
- Normal total and ionized calcium level
- Elevated PTH
- No other etiology for secondary hyperparathyroidism:
- Chronic kidney disease
- Vitamin D deficiency
- Medications
- Renal hypercalciuria
- Malabsorption syndromes
- The natural history of this variant includes:
- Stability or progression toward hypercalcemia.
- Uncommonly, patients with PHPT can present with hypercalcemic crisis:
- Which occurs when the serum calcium level is markedly elevated and often presents with symptoms of mental status changes.
- Treatment starts with:
- IV hydration with or without forced diuresis
- Followed by bisphosphonates.
- Some patients may require calcitonin, glucocorticoids, or even dialysis.
- 25-OH vitamin D level should be measured:
- Vitamina D deficiency is a common occurrence in classic PHTP (elevated calcium and elevated PTH).
- In patients with posible normocalcemic PHPT and a low 25 OH vitamin D level:
- Secondary hyperparathyroidism due to vitamin D deficiency should be rule out.
- Other laboratory values that could also be measured include:
- A serum phosphorus level,:
- Which is low or low normal in PHPT
- Alkaline phosphatase activity:
- Which when elevated, is an indication of more active bone disease.
- A 24-hour urine for calcium and creatinine is obtained:
- To rule out familial hypocalciuric hypercalcemia and assess for the presence of high urinary calcium excretion:
- If elevated, a stone risk profile is recommended.
- To rule out familial hypocalciuric hypercalcemia and assess for the presence of high urinary calcium excretion:
- A serum phosphorus level,:
- A bone density study may be useful in helping to determine the need for surgery.
- An abdominal film, CT, and MRI may identify asymptomatic nephrolithiasis but are not a routine part of the work-up.
- Sestamibi:
- The most widely used imaging study is the sestamibi scan:
- Identifies an abnormal parathyroid gland 60% to 90% of the time.
- The radioisotope is taken up by the thyroid and parathyroid glands and over time (45 to 90 minutes) washes out of the thyroid gland, leaving uptake in the enlarged parathyroid gland(s)
- Variations of the technique include:
- SPECT
- Subtraction using 99Tc pertechnetate thyroid scan
- SPECT-CT fusion:
- The study is useful in detecting mediastinal adenomas (the chest should always be imaged) and can obviate a neck exploration in small number of patients with mediastinal adenomas.
- The most widely used imaging study is the sestamibi scan:
- Limitations of sestamibi include:
- Low sensitivity for small adenomas and multiple gland disease.
- The addition of SPECT and SPECT-CT adds to anatomic definition.
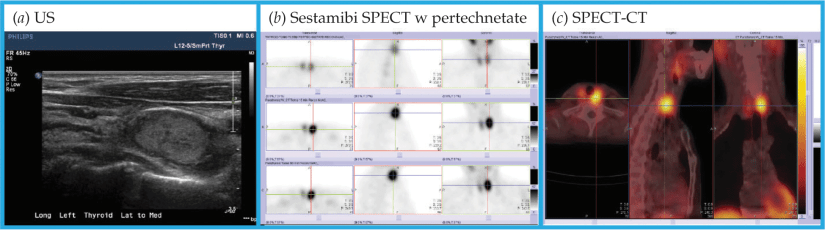
- Ultrasound:
- Neck ultrasonography is a complementary imaging study.
- The sensitivity ranges from 60% to 80% and provides more detailed anatomic information for operative planning.
- Ultrasonography also identifies concomitant thyroid pathology:
- Present in 30% to 50%:
- Which could be simultaneously addressed if necessary during parathyroidectomy.
- Present in 30% to 50%:
- 4D CT scan:
- Four-dimensional CT is a highly accurate and anatomically specific method of localizing parathyroid adenomas and may be superior to ultrasonography and sestamibi in detecting multiple gland disease.
- It captures images of the neck before, during, and after contrast infusion:
- Can distinguish between lymph nodes and abnormal parathyroid glands
- It subjects the patient to significant radiation exposure and contrast dye load.
- It is very useful in reoperative parathyroid surgery and has largely replaced selective venous sampling for localization in these difficult cases.
Rodrigo Arrangoiz MS, MD, FACS cirujano de tumores de cabeza y cuello / cirugía endocrina / cirugía oncológica miembro de Sociedad Quirúrgica S.C. experto en el manejo del hiperparatiroidismo:
Rodrigo Arrangoiz MS, MD, FACS es miembro de la American Thyroid Association:

Publicaciones sobre el hiperparatiroidismo:
-
Current Thinking on Primary Hyperparathyroidism
-
Does Vitamin D Deficiency Cause Primary
-
Primary Hyperparathyroidism and Thyroid Cancer: A Case Series
-
Parathyroid Embryology, Anatomy, and Pathophysiology of Primary Hyperparathyroidism
-
The return of the bilateral neck exploration for primary Hyperparathyroidism
Rodrigo Arrangoiz MS, MD, FACS cirujano de tumores de cabeza y cuello / cirugía endocrina / cirugía oncológica miembro de Sociedad Quirúrgica S.C. pionero en México de la paratiroidectomia radioguiada mínimamente invasiva:
Entrenamiento:
-
Cirugia general y gastrointestinal:
• Michigan State University: 2004- 2010




