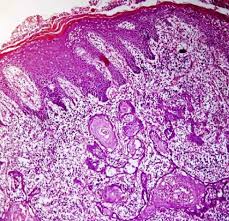
A. Squamous Cell Carcinoma:
– More than 90% of all head and neck cancers in the West are squamous cell carcinomas.
B. Histologic grade:
1. There are three histologic grades based on the amount of keratinization:
– A well-differentiated tumor is characterized by more than 75% keratinization.
– A moderately differentiated tumor, is characterized by 25% to 50% keratinization.
– A poorly differentiated tumor is characterized by less than 25% keratinization.
-
Histologic grade has not been a consistent predictor of clinical behavior.
C. Features that predict aggressive behavior include:
1. Perineural spread
2. Lymphatic invasion
3. Tumor spread beyond the lymph node capsule (Extranodal extension – ENE).
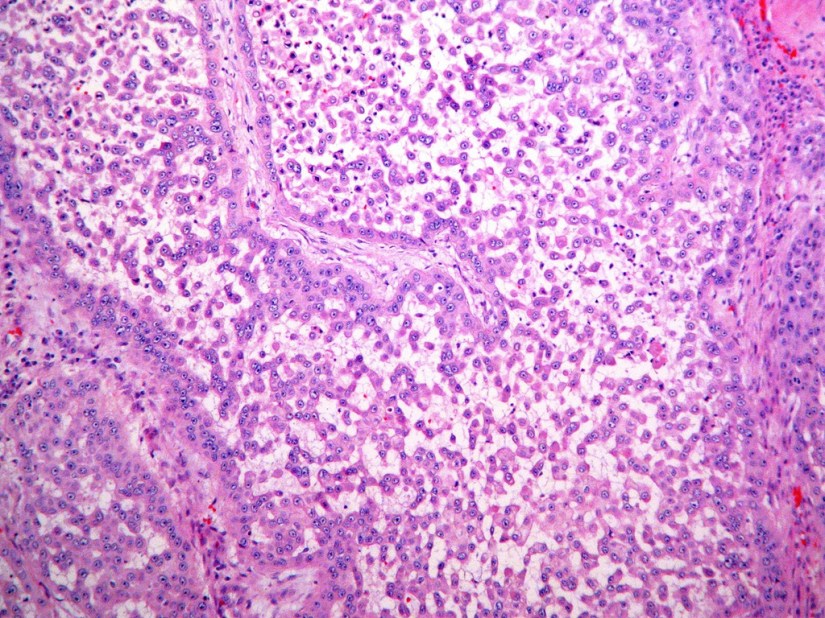
D. HPV-positive tumors tend to be non-keratinizing and poorly differentiated.
-
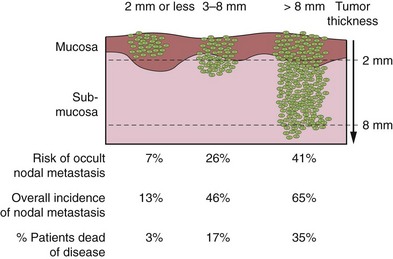
The most important histological feature of the primary tumor that affects selection of treatment and eventual prognosis is its depth of infiltration.
-
Thin and superficially invasive lesions have a lower risk of regional lymph node metastasis, are highly curable, and offer an excellent prognosis.
-
On the other hand, thicker lesions that deeply infiltrate the underlying soft tissues have a significantly increased incidence of regional lymph node metastasis and an adverse impact on prognosis.
-
-
The risk of lymph node metastasis and survival rates in relation to the thickness of the primary lesion for T1 and T2 squamous carcinomas of the oral tongue and floor of mouth are shown in the Figure.
-
Although it would be ideal to know the exact thickness of the lesion before surgical intervention, in many instances having that information before surgical excision of the primary tumor is clinically impractical.
-
In general, however, thickness of the lesion as appreciated by palpation is a reasonably good indicator of deeply invasive lesions versus superficial lesions to estimate the extent of soft tissue and/or bone resection for the primary lesion and to decide on the need for elective dissection of the regional lymph nodes at risk in a neck with negative clinical findings.
-
Pooled data from the literature on the thickness of the primary tumor for selection of elective treatment of the neck indicate that lesions thicker than 4 mm have a progressively increased risk of lymph node metastasis.
-
-
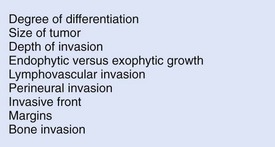
The presence of perineural invasion and the presence of lymphovascular tumor emboli are prognostic indicators for tumor control and survival.
-
Local recurrence also is affected by the pattern of tumor infiltration, with single cell infiltration more unfavorable than a broad, “pushing” border.
-
As one would expect, negative margins are another key factor in locoregional control.
-
If a tumor is present less than 5 mm from the resection margin, it should be stated in the pathology report because the presence of lesions (i.e., severe dysplasia/carcinoma in situ and invasive carcinoma) within this distance has been reported to be associated with a significant risk of local recurrence.
-
Histological features of the primary tumor that have an impact on therapeutic outcomes are shown in the figure.
-
-
Rodrigo Arrangoiz MS, MD, FACS a head and neck surgeon and is a member of Sociedad Quirúrgica S.C at the America British Cowdray Medical Center.
He is first author on some publications on oral cavity cancer:
-
Oral Tongue Cancer: Literature Review and Current Management
-
Understand Cancer: Research and Treatment Oral Cavity Cancer: Literature Review and Current Management.
Training:
• General surgery:
• Michigan State University:
• 2004 al 2010

• Surgical Oncology / Head and Neck Surgery / Endocrine Surgery:
• Fox Chase Cancer Center (Filadelfia):
• 2010 al 2012

• Masters in Science (Clinical research for health professionals):
• Drexel University (Filadelfia):
• 2010 al 2012

• Surgical Oncology / Head and Neck Surgery / Endocrine Surgery:
• IFHNOS / Memorial Sloan Kettering Cancer Center:
• 2014 al 2016

-