A. Hypocalcemia secondary to hypoparathyroidism
Reported rates of transient hypocalcemia vary in the medical literature from 5% to 50%, but the rate of permanent hypocalcemia secondary to hypoparathyroidism (ie, lasting more than 6 months) is below 3% (0.5% to 2%).
- The pathophysiology behind transient hypoparathyroidism and hypocalcemia is not well understood but is thought to be related to a transient ischemia to the parathyroid glands or perhaps an increased release of the acute phase reactant endothelin 1.
- A systematic review of predictors of post-thyroidectomy hypocalcaemia found perioperative parathyroid hormone (PTH), preoperative vitamin D and postoperative changes in calcium to be biochemical predictors.
- Patients who are at increased risk for this complication are those with Graves disease or malignancy or those undergoing total thyroidectomy, or total thyroidectomy with central compartment neck dissection.
Patients may initially be asymptomatic while hypocalcemic. Classic presenting symptoms include numbness and tingling of the digits or perioral area, carpopedal spasm, or the presence of a Chvostek sign or a Trousseau sign. In severe cases, patients may also experience tetany, EKG changes (QT prolongation), seizures, mental status changes, or cardiac arrest secondary to hypocalcemia.
- The Chvostek sign can be reproduced by tapping on the face just anterior to the ear, causing contraction of the ipsilateral facial muscles.
- A patient with a positive Trousseau sign will have spasm of the wrist, fingers, or thumb with inflation of a sphygmomanometer above the systolic blood pressure.
- Either sign is indicative of neuromuscular excitability associated with hypocalcemia.
Patients who are noted to have postoperative hypocalcemia should be managed with calcium supplementation. By following the trend of serum calcium levels, oral calcium supplementation can be titrated accordingly.
- If patients are receiving 2 grams of elemental calcium and continue to have decreasing or low serum calcium, calcitriol supplementation between 0.25 mcg to 1 mcg per day can be considered.
- Additionally, intravenous calcium replacement may be necessary for patients refractory to oral management or those with severe symptomatic hypocalcemia.
- Endocrinology consultation should be considered in these patients.
- Of note, serum calcium levels should be corrected for concurrent hypoalbuminemia and any hypomagnesemia should be medically corrected.
Patients who develop hypocalcemia should be discharged with calcium and vitamin D supplementation and if necessary calcitriol supplementation. After a few months, weaning from the calcium supplementation can be considered.
B. Injury to the recurrent laryngeal nerve
- Injury to the recurrent laryngeal nerve (RLN) can yield vocal fold paresis or paralysis. The implementation of nerve monitoring has not been proven to lower this risk, but may provide prognostic value.
- Studies show that identifying the RLN is associated with lower rates of injury (knowledge of anatomy).
- These cases may be underestimated, as not all patients undergo postoperative laryngeal evaluation.
- Should an injury occur, the patient usually presents with postoperative persistent hoarseness.
- Patients may also describe dysphagia or aspiration with thin liquids.
- Patients who undergo total thyroidectomy are at risk for bilateral vocal fold paralysis, a devastating complication.
- This usually manifests in the immediate postoperative period with airway obstruction, biphasic stridor, or respiratory distress.
Patients with suspected recurrent laryngeal nerve injury should be evaluated with flexible laryngoscopy or videostroboscopy to confirm the position and movement of the vocal folds.
- Should they have aspiration or dysphagia symptoms, they should be evaluated by a speech language pathologist.
- Patients with suspected bilateral vocal fold paralysis may require urgent and definitive airway management with a tracheotomy.
- At this point, any persistent injury may be considered permanent.
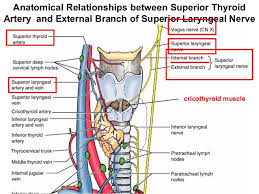
The superior laryngeal nerve has both an internal and external branch.
- The internal branch provides sensory innervation to the larynx (supra glottic larynx), while the external branch innervates the cricothyroid muscle.
- This posterior laryngeal muscle assists with lengthening of the vocal fold.
- Estimates of this complication vary, and are likely underestimated.
- Voice professionals, however, can be significantly affected by this injury, as it affects the ability to produce higher-pitched sounds and thus may affect a singer’s upper register.
This injury too may be evaluated videostroboscopy, as well as laryngeal electromyography (EMG):
- Some slight bowing of the affected vocal cord may be present, and the affected vocal cord may be lower than the normal cord.
- Additionally, EMG shows a deficit in the cricothyroid muscle.
D. Neck hematoma
A rare but but dangerous complication of thyroidectomy, neck hematomas can form secondary to inadequate hemostasis or a coagulopathy.
- Incidence of this complication is approximately 1%, but its occurrence can lead to asphyxiation and airway compromise.
- When identified on physical examination, the patient must be taken back to the operating room for exploration and achieving hemostasis.
- If the patient is in respiratory distress, the surgical wound should be opened and the hematoma evacuated immediately (even at the bedside) and then the patient should be taken to the operating room.

E. Infection
The rates of infection after thyroidectomy have significantly decreased with improvements in technology and aseptic technique and are currently estimated between 1% to 2%.
- The usual presentation is a superficial cellulitis with warmth, erythema, and tenderness surrounding the surgical incision.
- If fluctuance is present, a superficial abscess may also be present.
- Other signs of infection, such as fever and leukocytosis, without an overlying cellulitis, may point to a deep space neck infection or abscess.
- Abscess needs to be drained, and the aspirate should be sent for cultures.
- Patients with a superficial cellulitis need to be on antibiotics that cover gram-positive organisms, while those with abscesses should be placed on broad-spectrum antibiotics until cultures yield specific bacteria.
Drexel University
Sociedad Quirúrgica S.C.
Hospital ABC Santa Fé
Av. Carlos Graef Fernández #154
Col. Tlaxala, Delg. Cuajimalpa
México, D.F. 05300
Tel: 1103 – 1600 Ext 4515 a la 4517
Fax:1664 – 7164




